Download PDF
Healthy corneal epithelium is essential in protecting the eye against infection and structural damage to deeper tissues. A nonhealing, or persistent, epithelial defect occurs when there is a failure of the mechanisms promoting corneal epithelialization within the normal two-week time frame.1 In addition to causing compromised vision and ocular discomfort, nonhealing corneal epithelial defects can have other deleterious consequences, including infection, scarring, melting, and perforation.
Etiology
In order to initiate appropriate management, it is important to determine the etiology of the defect. The conditions that most commonly lead to a persistent epithelial defect fall into four major categories.1
- Epithelial/limbal stem cell deficiency constitutes a category of conditions in which epithelial cells are shed but not adequately replaced.
- Inflammatory disease, including keratoconjunctivitis sicca, may accompany any of the other conditions.
- Neurotrophic disease, which impairs corneal sensation, is often a major culprit. Common causes include diabetes, past or present herpetic infection, and nerve damage from laser or incisional ocular surgery.
- Mechanical factors, especially abnormal lid pathology, can lead to epithelial trauma, ocular surface disease, and limbal stem cell attrition.
 |
|
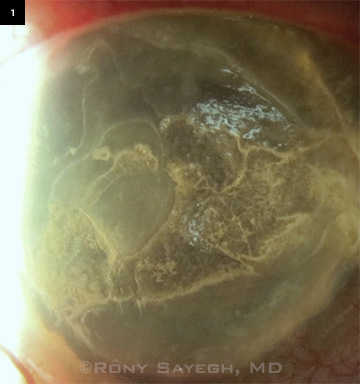
NONHEALING DEFECT. Persistent corneal epithelial defect resulting from band keratopathy.
|
Management
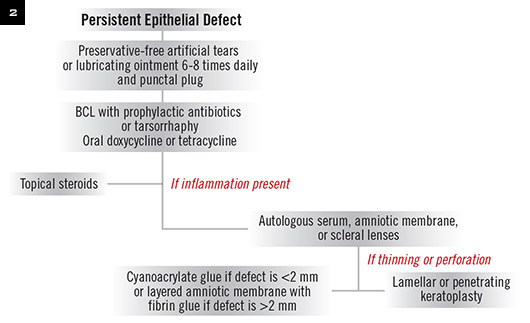
Treatment of a persistent epithelial defect is based upon the clinical condition of the epithelium at presentation as well as the underlying etiology. For example, the defect in Figure 1 was managed by treating the underlying band keratopathy with EDTA chelation. Most cases will resolve with a stepwise management strategy, as outlined in this article (Fig. 2).
Lubrication. The first step involves support of the ocular surface with aggressive lubrication using preservative-free artificial tears or lubricating ointment every one to two hours.
Punctal plugs. We encourage early use of punctal occlusion to increase the retention of natural tears, which facilitates the healing process.1,2 However, it is important to consider the etiology before doing so; if used in severe inflammatory disorders, punctal plugs can exacerbate both the epithelial defect and the underlying condition.
In our practice, we typically start with a silicone plug in the lower punctum. Alternatively, temporary collagen plugs, thermocautery, argon laser, or electrocautery can be employed.
Bandage contact lens (BCL). Soft therapeutic contact lenses serve to protect the corneal surface from mechanical trauma from the eyelids. A soft contact lens with high oxygen permeability (such as a silicone hydrogel) may be chosen to reduce complications such as corneal edema and neovascularization.2 In our experience, a 16- or 18-mm Kontur lens (Kontur Kontact Lens) is often effective; its diameter is greater than the limbal margin, and its thickness provides stability. Ointments should be discontinued for patients using a BCL.
It takes approximately seven days after the epithelium heals for adhesions to form. However, if the stroma is involved, it may take eight weeks or more for epithelial cells to adhere to the underlying basement membrane/stroma.1,2 It may be desirable to keep the BCL in the eye for approximately one week after the epithelium heals, but BCLs are sometimes kept in place for as long as two or three months. The risk of infection from longer use should be weighed against the risk of recurrence of the defect.
Tarsorrhaphy. Tarsorrhaphy involves partial or complete closure of the eyelid fissure to allow the ocular surface to heal itself. This minor in-office procedure can be a very effective treatment for persistent epithelial defect, and it avoids the risk of infection associated with use of a BCL. It may be particularly useful for noncompliant or debilitated patients who are unreliable in carrying out conservative management methods, as well as for patients in whom lagophthalmos or exposure keratopathy contributes to defect formation.1,2
Using bolsters and sutures through the tarsus/lid margin is the preferred method for tarsorrhaphy (see Ophthalmic Pearls, EyeNet, April 2014). Antibiotic ointment is applied to the eye and on the sutures after the procedure is performed. Alternatively, cyanoacrylate glue can be applied to the eyelashes to close the fissure. Tarsorrhaphy may be used as a temporary measure lasting up to several weeks or as a permanent solution in severe cases. However, patients are seldom pleased with cosmesis after tarsorrhaphy.
Tetracyclines. If there are no contraindications, oral tetracyclines, which have anticollagenolytic properties, may aid in corneal wound healing and prevent stromal lysis. Oral tetracycline (250 mg four times daily) and doxycycline (20-100 mg twice daily) have each demonstrated benefits in patients with persistent epithelial defects.1-3
Prophylactic topical antibiotics. Although the risk of infection in an eye with a persistent epithelial defect is low, many experts advocate the use of polymixin B–trimethoprim (e.g., Polytrim) or a fourth-generation fluoroquinolone two to four times daily for prophylaxis. If a BCL is in place, prophylactic topical antibiotics should always be used.3
Steroids. Corticosteroid use remains controversial in the management of persistent epithelial defects.3 However, a small amount of inflammation invariably seems to be present, hindering normal epithelial healing.1-3 Application of topical steroids such as loteprednol or prednisolone twice daily tends to be very helpful. Loteprednol is the only topical ophthalmic steroid ointment commercially available in a nonpreserved form; other steroids can be compounded to be preservative free.
Refractory Cases
If response to the previous measures is inadequate, the following therapies may be helpful.
Amniotic membrane grafting. Human amniotic membrane contains several factors that promote epithelial wound healing.1-3 Amniotic membrane patches can be either glued or sutured in place or positioned under a BCL. In addition, amniotic membrane is commercially available within a PMMA ring (Prokera; Bio-Tissue) that is placed in the eye like a contact lens.
Autologous serum. Autologous serum drops have been reported to be beneficial in the treatment of persistent epithelial defect recalcitrant to conventional therapy. The patient’s serum is diluted to a concentration of 20 percent, and the drops are used six to eight times daily.4 The therapeutic effect is promoted by various growth factors contained in the serum, including vitamin A, substance P, immunoglobulins, and fibronectin.4
Although most studies, as well as our own clinical experience, have shown favorable results and few complications with autologous serum, several factors limit its use in clinical practice. These include cost, the need for blood draws, and a lack of familiarity with this approach among clinicians.4 No blood should be taken from patients with suspected septicemia. To reduce the risk of viral transmission to third parties, treatment with autologous serum should not be performed in patients testing positive for HIV, hepatitis type B or C, or syphilis.
Umbilical cord serum has also been investigated as an alternative and may promote even faster healing.5
Scleral contact lenses. Scleral lenses, including the prosthetic replacement of ocular surface ecosystem (PROSE) lens, may be utilized for refractory persistent epithelial defects. Such lenses vault over the cornea to protect the ocular surface and provide a reservoir for hydration. In a recent report, the extended-wear PROSE lens coupled with a nonpreserved fourth-generation fluoroquinolone in the device reservoir resulted in healing of persistent epithelial defects with reduced rates of microbial keratitis.6
 |
|
MANAGEMENT APPROACH. Suggested treatment flow diagram for persistent corneal epithelial defect. (BCL, bandage contact lens.)
|
Thinning and Perforation
Cyanoacrylate glue. If the defect progresses to severe thinning and impending perforation, cyanoacrylate glue may promote epithelialization and halt progression. The glue is useful in cases of perforations less than 2 mm and has significantly reduced the need for keratoplasty.7
Amniotic membranes. Multilayer amniotic membranes with human fibrin glue have been shown to promote re-epithelialization in larger defects while increasing tissue thickness. This method is a good alternative to avoid or delay corneal transplantation when the risk of graft rejection is high.
Keratoplasty. Corneal transplantation is reserved for severe cases and should be performed only after three to six months of clinical stability. Concurrent amniotic membrane placement and/or a temporary tarsorrhaphy should be used to aid in healing.8
For small- to intermediate-sized perforations, lamellar grafts have the advantage of lower rejection rates, faster healing times, and preservation of endothelium compared with penetrating keratoplasty.9 However, worse visual outcomes are often seen after lamellar transplants unless Descemet’s membrane is bared. Great care must be taken after these procedures, since postoperative delay in epithelial healing can lead to poor wound healing and risk of melt and infection.
Keratoprosthesis. A keratoprosthesis may be tried as a last resort to maintain visual functioning in the absence of a healthy epithelium.
Novel Treatments
Several therapies are currently in the pipeline for treatment of persistent epithelial defects.
Fibronectin. Fibronectin is a naturally occurring glycoprotein found in serum that promotes cellular adhesion in wound healing. Conflicting reports in the literature about topical fibronectin’s benefits in the treatment of persistent epithelial defects have limited its clinical use for this condition.10
Thymosin beta 4. Tβ4, a naturally occurring polypeptide secreted by inflammatory cascade cells, plays an active role in promoting corneal wound healing. In a recent case series, topical, nonpreserved ophthalmic Tβ4 known as RGN-259 (RegeneRx Biopharmaceuticals) showed promising results in the treatment of nonhealing neurotrophic epithelial defects.11 It has recently obtained orphan drug designation from the U.S. Food and Drug Administration.
Nexagon. The active ingredient in topical Nexagon (CoDa Therapeutics) is a natural antisense oligonucleotide that decreases connexin43 expression levels and dampens the inflammatory response. Topical ophthalmic Nexagon gel has shown encouraging results in the treatment of alkali corneal burns.12 It is currently undergoing phase 2 clinical trials in patients with persistent epithelial defects in New Zealand and the United States.
___________________________
1 Dahlgren MA et al. Persistent epithelial defects. In: Albert DM, Miller JW, eds. Albert & Jakobiec’s Principles and Practice of Ophthalmology. Philadelphia: Elsevier; 2008:749-759.
2 Tuli SS et al. Ocul Surf. 2007;5(1):23-39.
3 Chang BH et al. Neurotrophic keratitis. In: Krachmer JH et al., eds. Cornea. Philadelphia: Elsevier; 2011:1101-1108.
4 Young AL et al. Eye (Lond). 2004;18(6):609-614.
5 Vajpayee RB et al. Br J Ophthalmol. 2003;87(11):1312-1316.
6 Lim P et al. Am J Ophthalmol. 2013;156(6):1095-1101
7 Webster RG et al. Arch Ophthalmol. 1968;80(6):705.
8 Hick S et al. Cornea. 2005;24(4):369-377.
9 Hirst LW et al. Ophthalmology. 1982;89(6):630.
10 Phan TM et al. Am J Ophthalmol. 1987;104(5):494-501.
11 Dunn SP et al. Arch Opthalmol. 2010;128(5):636-638.
12 Ormonde S et al. J Membr Biol. 2012;245(7):381-388.
___________________________
Dr. S. Gupta is a third-year ophthalmology resident; Dr. P. Gupta and Dr. Sayegh are assistant professors of ophthalmology specializing in cornea and refractive surgery; all are at University Hospitals Case Medical Center in Cleveland, Ohio. The authors report no related financial interests.