By Linda Roach, Contributing Writer, interviewing Jennifer I. Lim, MD, Lucia Sobrin, MD, MPH, and Andre J. Witkin, MD
Download PDF
Fearful of postoperative endophthalmitis, many cataract surgeons in the United States have added intracameral vancomycin to their surgical routines over the last decade.1,2 But the discovery of a link between vancomycin and a rare, catastrophic disease entity known as hemorrhagic occlusive retinal vasculitis (HORV) has raised doubts about the use of this antibiotic for intracameral surgical prophylaxis.
Although causation has not been proved, HORV is thought to stem from a type III hypersensitivity reaction to intraocular vancomycin. The condition manifests painlessly as a sudden, dramatic decrease in visual acuity, with retinal vascular occlusions, numerous peripheral hemorrhages, and ischemia. Reports to date indicate that this occurs from 1 to 26 days after uneventful cataract surgery.
This delayed presentation led to devastating visual losses in patients with HORV who underwent second- eye cataract surgery before the first eye became symptomatic, said Andre J. Witkin, MD, at the New England Eye Center in Boston. Dr. Witkin is part of a physician task force investigating HORV cases around the nation.
“This disease is really terrible. In some cases, people had their second surgery within a week or two of the first, and only after the second surgery did the disease manifest—and they ended up going blind in both eyes,” he said.
 |
|
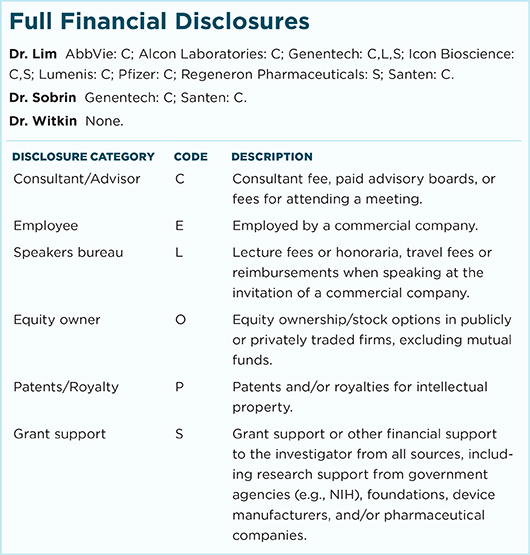
RIGHT EYE. A 66-year-old woman presented with decreased vision 10 days after otherwise uncomplicated bilateral sequential cataract surgery spaced 1 week apart. Intracameral vancomycin (1 mg/0.1 cc) was used at the end of each case. The right eye surgery was first. Despite treatment with systemic corticosteroids and valacyclovir, the patient developed neovascular glaucoma, and her visual outcome was NLP. (1A) The mosaic color photograph demonstrates diffuse peripheral retinal vascular occlusion and associated large patches of retinal hemorrhage. Ischemic macular whitening is evident. The retinal veins are not tortuous or dilated. (1B) Fluorescein angiography (FA) reveals retinal vascular occlusion in areas of retinal hemorrhage. (1C) Optical coherence tomography (OCT) shows a thickened macula and hyperreflectivity of the inner retinal layers, indicating ischemia. Cystoid macular edema is not prominent.
|
Investigating HORV
In 2015, Dr. Witkin and his colleagues published a case series describing the first 6 known patients with HORV (in 11 eyes).3 In that report, intracameral vancomycin was the only risk factor in common among all the affected eyes. (No single formulation or manufacturer was implicated.)
Subsequently, a task force convened by the American Society of Cataract and Refractive Surgery (ASCRS) and the American Society of Retina Specialists (ASRS) established a registry (www.asrs.org, click “Report HORV Incidents Here”) and learned of additional cases, for a total of 36 eyes in 22 patients.4 Of these, 14 patients had bilateral disease. Visual acuity was 20/200 or worse in 22 eyes (61%), and 8 eyes (22%) had no light perception (NLP).
When will there be good news? As bad as those reports are, the task force analysis and smaller case studies also contain some good news about HORV.
- Early signs. The disease appears to have a wide clinical spectrum, suggesting an opportunity for clinicians to prevent profound vision loss by recognizing early, sometimes nonhemorrhagic signs of a hypersensitivity reaction4-6 (see “In the Clinic,” below).
- Treatment strategy. Severe vision loss might be prevented with intensive topical, oral, and intravitreal corticosteroids; intravitreal anti-VEGF injections to prevent rapid development of neovascular glaucoma; and panretinal photocoagulation (PRP) to stabilize the retina4,5 (see “Treatment Guidance,” below).
Why now? Investigators have been unable to explain why HORV is showing up only now, said Lucia Sobrin, MD, MPH, at Massachusetts Eye and Ear in Boston. “Ophthalmologists have been using intravitreal [injections of] vancomycin for endophthalmitis for years, without reports of this problem.”
However, some observers wonder whether hidden HORV did occur in the past, when ophthalmologists were treating bacterial endophthalmitis with vancomycin, said Jennifer I. Lim, MD, at the University of Illinois at Chicago. “I remember seeing some eyes after intravitreal antibiotic injections for endophthalmitis where there was quite a lot of hemorrhaging, and we said, ‘Oh, this is from the endophthalmitis,’” Dr. Lim said. “But maybe, in some cases, the hemorrhage we saw might have been from the vancomycin and we just never knew it, because the vitreous was completely whited out and we could not see the retina prior to treatment. We’ll never really know.”
 |
|
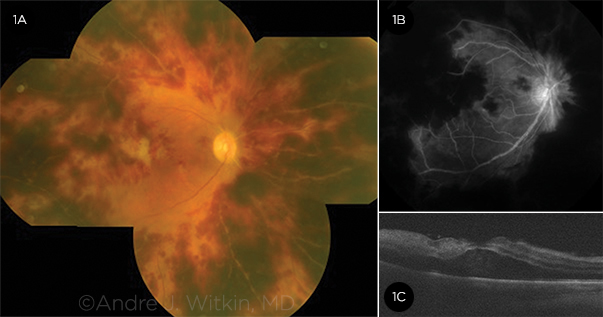
LEFT EYE. The patient’s second eye became symptomatic 1 week after the first. She received anti-VEGF injections and PRP for neovascular glaucoma, in addition to systemic corticosteroids early in the disease course. Her visual outcome was 20/200. (2A) The mosaic color photograph demonstrates peripheral retinal vascular occlusion with large patches of retinal hemorrhage. There are 2 cotton-wool spots in the macula, but the macula appears otherwise normal. The retinal veins are not tortuous or dilated. (2B) FA reveals retinal vascular occlusion in areas of retinal hemorrhage. Staining of retinal venules is evident. (2C) OCT shows mild hyperreflectivity in the inner retinal layers, indicating macular ischemia.
|
Immunologic Clues to HORV
According to the ASCRS/ASRS Clinical Alert, there is evidence of a “strong association” between HORV and intra-cameral vancomycin use, possibly resulting from a type III hypersensitivity reaction.4
In type III hypersensitivity, exposure to an antigen leads to antibody production, and these antibodies bind to the antigen in the circulation, Dr. Sobrin said. “These antibody-antigen complexes are deposited in vessel walls, and then an inflammatory cascade goes along from there. Thrombi also form in the vessels, leading to ischemic injury,” she said. “If the immune system has previously ‘seen’ the precipitating antigen, the reaction can happen very quickly and severely.”
Initial hint. In 2014, Dr. Sobrin and her colleagues (including Dean Eliott, MD, Thomas A. Albini, MD, Andrew A. Moshfeghi, MD, and Carmen Santos, MD) published the first report on ischemic retinal vasculitis after cataract surgery with vancomycin.7
“One of the 2 patients in our study had a documented reaction to vancomycin with renal failure previously. That was one of the main reasons that vancomycin hypersensitization came to our attention,” she said.
Direct toxicity ruled out. Initially, there was speculation that an adjuvant given during surgery, either alone or in combination with the vancomycin, was directly toxic to retinal vessels, Dr. Witkin said.
However, patients who developed HORV had good visual acuity on postop day 1. Visual deterioration was delayed, ranging from 1 to 26 days postoperatively (mean, 8 days).4 “We would expect toxicity to occur immediately after surgery,” Dr. Witkin said. In addition, other studies “haven’t shown vancomycin to be toxic to the eyes in animals, unless it’s given in really high doses,” he said.
Echoes of other immune diseases. HORV presents similarly to leukocytoclastic vasculitis and Henoch-Schönlein purpura, which are type III hypersensitivity reactions in the skin associated rarely with vancomycin.4
“Leukocytoclastic vasculitis has a delayed presentation of 1 to 2 weeks, and it tends to affect veins, and that’s what we saw in our HORV patients,” Dr. Witkin said. “The veins were strikingly affected, out of proportion to the arterioles. There were a lot of hemorrhages surrounding the veins, and the veins were sheathed in a lot of cases.”
Dr. Sobrin agreed. “Type III sensitivity reactions typically affect the small venules, the postcapillary venules, and that’s what we see in HORV.”
Dose-response relationship. Greater exposure to vancomycin in the affected eyes correlated with greater disease severity, suggesting a dose-response relationship.
This was tragically apparent in 7 eyes that, before HORV was recognized, were treated presumptively for suspected bacterial endophthalmitis—with intravitreal injections of vancomycin. Five of these 7 eyes were NLP at the most recent follow-up.4
“Conversely, there was a patient who had a much lower dose of vancomycin in the infusion bottle, and this person only had a mild reaction,” Dr. Witkin said. “There were hemorrhages and vascular occlusions, but the condition resolved on its own without treatment.”
Treatment Guidance
Considerations for using prophylactic vancomycin:
- Weigh the potential risk of HORV, which is extremely rare, against the risk of endophthalmitis.
- Reconsider using vancomycin with close sequential bilateral cataract surgery.
- If using vancomycin with sequential cataract surgery, remember that HORV has delayed onset; further, it may be asymptomatic in the first eye and detectable only with a dilated retinal exam.
- Cefuroxime or moxifloxacin may be alternatives for intracameral prophylaxis.
Recommendations for managing HORV:
- Consider avoiding intravitreal vancomycin if both bacterial endophthalmitis and HORV are in the differential diagnosis.
- Consider an ocular and/or a systemic workup for other syndromes (e.g., viral retinitis).
- Aggressively use systemic and topical corticosteroids; consider periocular or intraocular steroids.
- Employ early anti-VEGF treatment.
- Employ early PRP.
SOURCE: Adapted from Clinical Alert: HORV Association With Intraocular Vancomycin.
|
In the Clinic
Early recognition of HORV in cataract patients who received vancomycin is crucial to preserving as much retinal function as possible, the experts say. If a cataract surgeon is using intracameral vancomycin and close sequential second-eye surgery is planned, or if a patient who saw well 1 day after surgery suddenly experiences decreased vision, a dilated examination should be done to look for vasculitis and intraretinal hemorrhages, Dr. Witkin said.
Recognize first. Some reports5,6 suggest that HORV has a wide spectrum of severity, including mild or even asymptomatic disease that can resolve if addressed promptly with topical and oral steroids. “It is important to recognize this entity immediately when the patient presents. You shouldn’t waste time treating them for other things,” Dr. Sobrin said.
- HORV vs. endophthalmitis. Eyes with HORV look very different from those with endophthalmitis, Dr. Witkin said. “In HORV, there’s a fairly clear view to the retina, with relatively little anterior chamber reaction or vitritis. That distinguishes it from endophthalmitis, where a lot of the time you don’t have a view of the retina at all,” he said. “With HORV, the retinal findings are really out of proportion to the amount of inflammation in other parts of the eye.”
Treat promptly. For fulminant cases, treatment should be immediate and aggressive to limit the amount of vision lost to severe retinal ischemia.4 Strategies include 1) topical, oral, and, in some cases, periocular or intravitreal steroids to halt inflammatory processes inside the eye; 2) early use of intravitreal anti-VEGF to block the rapid development of neovascular glaucoma; and 3) early panretinal photocoagulation4 (see “Treatment Guidance” for further considerations).
In a case described last year, aggressive therapy partially reversed extreme vision loss in one eye of a bilateral HORV patient.5 Treatment consisted of topical Pred Forte (prednisolone 1%) and oral prednisone 50 mg daily, and 2 injections, given 1 month apart, of intravitreal bevacizumab. The patient initially presented with visual acuity of counting fingers in one eye and NLP in the other; after treatment, she improved to 20/80 in the first eye and counting fingers in the second.
Last but not least. Above all, be wary of using vancomycin if there is any hint that the eye might have HORV. “In terms of what to do in an eye that might have HORV, it is important to avoid using intravitreal vancomycin for suspected endophthalmitis,” Dr. Witkin said.
___________________________
NEXT MONTH. Should cataract surgeons stop using intracameral vancomycin altogether?
___________________________
1 Chang DF et al. J Cataract Refract Surg. 2007;33(10):1801-1805.
2 Chang DF et al. J Cataract Refract Surg. 2015;41(6):1300-1305.
3 Witkin AJ et al. Ophthalmology. 2015;122(7):1438-1451.
4 ASCRS-ASRS HORV Task Force. Clinical Alert: HORV Association With Intraocular Vancomycin. July 20, 2016. Accessed Dec. 13, 2016.
5 Ehmann DS et al. Retin Cases Brief Rep. Published online Aug 22, 2016.
6 Lenci LT et al. Case Rep Ophthalmol Med. 2015;2015:683194. doi:10.1155/2015/683194.
7 Nicholson LB et al. Ophthalmic Surg Lasers Imaging Retina. 2014;45(4):338-342.
___________________________
Dr. Lim is professor of ophthalmology and director of the Retina Service at the Illinois Eye and Ear Infirmary at the University of Illinois at Chicago, where she also holds the Marion H. Schenk, Esq., Chair in Ophthalmology for Research of the Aging Eye. Relevant financial disclosures: Alcon Laboratories: C; Pfizer: C; Santen: C.
Dr. Sobrin is attending physician and clinician scientist at Massachusetts Eye and Ear and associate professor of ophthalmology at Harvard Medical School in Boston. Relevant financial disclosures: None.
Dr. Witkin is assistant professor of ophthalmology and director of clinical research at the New England Eye Center at Tufts Medical Center in Boston. Relevant financial disclosures: None.
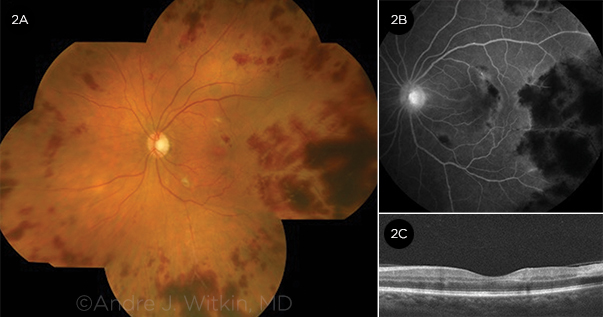
For full disclosures and the disclosure key, see below.