By Mike Mott, Contributing Writer, interviewing Neeru Gupta, MD, PhD, MBA, Sunita Radhakrishnan, MD, and Alan L. Robin, MD
Download PDF
A leaking filtration bleb is a common complication of trabeculectomy that can occur days, months, or years after the initial surgery. It’s also a vision-threatening danger that shouldn’t be ignored.
The bottom line: There should be no delay when addressing any type of bleb leak, said Neeru Gupta, MD, PhD, MBA, at the University of Toronto. “If the leak does not seal, the patient will have fluid leaving the eye, which can drop the pressure and lead to a whole host of complications.” Moreover, she pointed out, “the leaking eye has no barrier to the outside world and, suddenly, it’s open season for pathogens.”
Thus, “It’s really important to see each leaking bleb as a ticking time bomb,” Dr. Gupta said. “Yes, the bleb surgery can be technically challenging, but the general ophthalmologist has a critically important role to play. Although a glaucoma specialist may be involved in fixing the [actual] leak, it’s imperative that every ophthalmologist knows how to read the signs of what can be a very sight-threatening condition.”
A Faulty Filter
The conjunctival tissue of a bleb can become thinned and cystic due to the constant flow of aqueous, and the thinnest and most avascular areas are most susceptible to developing a leak.
This leakage can result from the surgical technique and/or the nature of the conjunctival tissue itself. “Early-onset bleb leakage occurs in the immediate period following surgery,” said Sunita Radhakrishnan, MD, at the Glaucoma Center of San Francisco. “There might be a leak at the incision site due to incomplete conjunctival closure or wound dehiscence, for example. Or the surgeon might have created an inadvertent opening in the conjunctival tissue.” The area where the bleb is most elevated can also develop a leak due to drying or microtrauma from repeated blinking.
Late-onset bleb leakage, on the other hand, is typically the result of thin bleb tissue. “The biggest reason a patient would develop this type of avascular tissue is the use of antifibrotics,” Dr. Radhakrishnan said. “Mitomycin C and 5-fluorouracil are commonly used as adjunctive treatment in filtering surgery to help prevent fibrosis and scarring. Although this can increase the survival of a filtering bleb, it can also result in more fragile tissue that is prone to leakage in the future.”
Danger, Danger
Regardless of when the leakage occurs, “A leaking bleb is not a minor issue,” said Alan L. Robin, MD, at the University of Michigan in Ann Arbor and John Hopkins University in Baltimore. “Early detection and management can help prevent serious complications.”
Potential complications. “If left untreated, the leak can lead to hypotony, which can result in a shallow or flat chamber, peripheral anterior synechiae, hypotony maculopathy, choroidal effusion, corneal striae, or even bleeding and surgical failure,” Dr. Robin said.
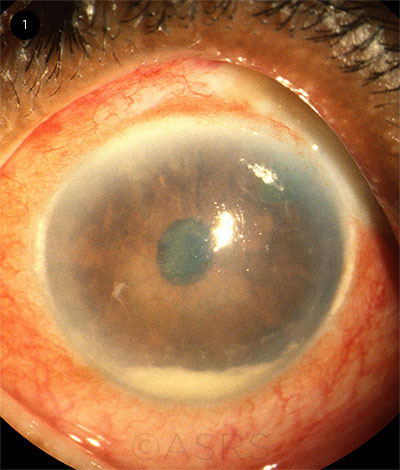
Risk of infection. “Bleb-related infection is a very dangerous and volatile situation if not managed promptly,” Dr. Gupta emphasized. “An open barrier in the ocular surface exposes the eye to any number of pathogens and microorganisms, so there’s a serious risk of intraocular infection. This can range from blebitis, an infection in or around the bleb without vitreous involvement, to endophthalmitis [Fig. 1].”
Signs of trouble. The surgeon can usually monitor for early-onset bleb leaks during surgery or in the immediate postoperative period.
After this point—and during normal follow-up—common signs of bleb leakage include a newly tearing eye, a noticeable change in vision, redness, or a drop in intraocular pressure (IOP) from baseline. “If you suspect a patient might have a leak, perform a Seidel test at the slit lamp to confirm,” said Dr. Gupta. “After painting the conjunctiva with a fluorescein strip under cobalt blue light, you’ll see the leak in the form of a greenish fluid escaping from behind the brown stain.”
Referral. “The bleb should be examined at every visit,” Dr. Robin said. “If a leak is present, given the potential serious sequelae, it should be addressed immediately.”
 |
|
ENDOPHTHALMITIS. Three years after undergoing trabeculectomy, this patient presented with pain, redness, and loss of vision in the left eye. This image was originally published in the ASRS Retina Image Bank. Ronald C. Gentile, MD. Bleb-Related Endophthalmitis. Retina Image Bank. 2012; Image Number 1764. © The American Society of Retina Specialists.
|
Stopping the Flow
Bleb leaks can resolve spontaneously, but if they don’t, what’s the fix? Treatment depends largely on your patient’s needs and how they present.
Medical treatment. “Conservative management is my first-line approach,” said Dr. Radhakrishnan, “especially if the leak is small with no infection, the visual acuity and pressure are stable, and the patient has no past history of bleb-related infection. Initially, I’ll use aqueous suppressants alongside prophylactic antibiotics to protect against infection. As long as the eye is stable and the bleb leak is decreasing, this approach can be followed until complete resolution in many cases.”
Other conservative approaches include:
- Direct pressure patching
- Bandage contact lens
- Collagen shields
- Autologous blood injections
- Compression sutures
- Cyanoacrylate glue
Surgical treatment. “There’s no hard-and-fast rule as to when you need to fix a bleb leak surgically,” Dr. Robin said. “But if the leak is not responding to initial management—or is brisk enough to cause corneal decompensation—or if the patient has experienced repeated episodes of bleb-related infection, definitive treatment always requires surgical repair.”
Although there is no gold standard for bleb leak repair, the common goal in the various surgical techniques is to cover the filtration site with healthy conjunctiva. The unhealthy bleb tissue is usually denuded or excised.
“Conjunctival advancement is 1 technique of bleb repair that entails covering the leaking bleb with a new flap of healthy conjunctival tissue that is advanced from the region posterior to the bleb,” said Dr. Radhakrishnan. “I typically remove the tissue that is leaking or ischemic. If there is not enough healthy conjunctiva for this approach, then a free conjunctival autograft from either the same eye or the fellow eye can be used.”
To test the bond after tacking down the advancement, Dr. Robin will inject balanced salt solution into the anterior chamber to check for any leakage and then confirm the result with a fluorescein test.
Learning curve. “Repairing a bleb leak surgically is not a particularly easy fix,” said Dr. Gupta. “Suturing through an avascular bleb that is already thin and friable—even with a fine suture like 10-0 nylon—can be challenging. The tissue may be as delicate as wet tissue paper, and punching holes in it can be like operating on Saran Wrap: One hole creates another even larger one.”
Because of these difficulties, ophthalmologists are continually searching for innovative ways to achieve the same results. “The patient might have unhealthy conjunctiva lacking useable tissue,” said Dr. Gupta. “For example, there might be too much scarring to perform a successful bleb revision. To fill these gaps, ophthalmologists have experimented with different patch graft materials other than conjunctiva, such as corneal tissue, amniotic membranes, mucosa from inside the cheek, and even fascia. It’s a struggle to manage aggressive bleb leakages, so we’re always looking for better ways.”
Postoperative Complications
Although positive outcomes are typically high for bleb repair, the clinician should expect that a few patients will develop complications, Dr. Radhakrishnan said.
The primary concern, she noted, is disturbing the preexisting aqueous flow. “Once you’ve repaired a leak, the conjunctiva is now thicker, so the pressure-lowering efficacy of the original trabeculectomy can decrease. You might see an early postoperative pressure spike from closing the bleb leak, or a slow rise in pressure over time as the bleb function slowly decreases. In our study, for example, 9% of patients required additional glaucoma surgery anywhere from 2 months to 7 years following bleb revision.”
Aside from glaucoma control, there are a few other—and less common—complications to be mindful of, said Dr. Gupta. These include hypertropia, ptosis, and dysesthesia. “When we’re performing advancement surgery, we are tugging on tissue from behind the upper lid close to the muscle and pulling it forward. This can result in muscle misalignment and drooping of the eyelid. And because the advanced conjunctiva might not sit flat at the limbus, the patient may experience eye discomfort when blinking.”
Risk of another leak. Of course, the patient might also develop another leak, she added. “There might also be something about the quality of the patient’s conjunctiva that predisposes it to leakage, and, voila, after plugging 1 hole, you’ve got another, and you have to treat all over again.”
___________________________
Dr. Gupta is professor of ophthalmology and chief of the Glaucoma Service at the University of Toronto, professor at the university’s Dalla Lana School of Public Health, and the Dorothy Pitts Chair of Ophthalmology and Vision Science at St. Michaels’ Hospital in Toronto. Relevant financial disclosures: None.
Dr. Radhakrishnan is a glaucoma specialist at the Glaucoma Center of San Francisco and research director of the Glaucoma Research and Education Group in San Francisco. Relevant financial disclosures: None.
Dr. Robin is professor of ophthalmology at the University of Michigan in Ann Arbor, Mich., associate professor of ophthalmology at the Wilmer Eye Institute in Baltimore, and associate professor of international health at Johns Hopkins Bloomberg School of Public Health in Baltimore. Relevant financial disclosures: None.
For full disclosures and the disclosure key, see below.
Full Financial Disclosures
Dr. Gupta Alcon: L; Canadian Institute of Health Research: S; Glaucoma Research Society of Canada: S.
Dr. Radhakrishnan Netra Systems: C,O.
Dr. Robin Aerie: C; Novaliq: C; Superior Vision: C.
Disclosure Category
|
Code
|
Description
|
| Consultant/Advisor |
C |
Consultant fee, paid advisory boards, or fees for attending a meeting. |
| Employee |
E |
Employed by a commercial company. |
| Speakers bureau |
L |
Lecture fees or honoraria, travel fees or reimbursements when speaking at the invitation of a commercial company. |
| Equity owner |
O |
Equity ownership/stock options in publicly or privately traded firms, excluding mutual funds. |
| Patents/Royalty |
P |
Patents and/or royalties for intellectual property. |
| Grant support |
S |
Grant support or other financial support to the investigator from all sources, including research support from government agencies (e.g., NIH), foundations, device manufacturers, and/or pharmaceutical companies. |
|