By Nicola Parry, Contributing Writer, interviewing K. David Epley, MD, R. Michael Siatkowski, MD, and Donald Tan, MD, FRCS, FRCOphth
Download PDF
For most people with myopia, the condition has only refractive ramifications. But those with high myopia are at risk for ocular pathology. (High myopia has recently been defined as –5.0 D or worse.1) Thus, the rising prevalence of myopia—which affects about 35% of the U.S. population aged 40-492—may mean an increasing number of high myopes who are at risk for developing associated serious eye diseases, ranging from choroidal neovascularization to glaucoma and retinal detachment, said K. David Epley, MD, in private practice in Kirkland, Wash.
Evidence builds. Because of growing concern about pathological myopia, recent research studies focused on slowing progression of garden-variety myopia in children have garnered interest among ophthalmologists. Low-dose atropine (0.01%) has emerged as an effective approach, as highlighted by the Atropine in the Treatment of Myopia studies (ATOM1 and ATOM2).3-7 Although ATOM enrolled Asian patients, studies are now under way involving other populations. A recent retrospective study in the United States included mostly Caucasian and Hispanic children.8 “This study suggests that atropine seems to work in various ethnic groups,” said Donald Tan, MD, FRCS, FRCOphth, at the Singapore National Eye Centre, and lead author of the ATOM studies.
Noting that other treatments to slow the progression of myopia, such as orthokeratology and soft contact lenses with peripheral defocus–modifying designs, may be inconvenient or have unwanted side effects, Dr. Epley described low-dose atropine as a significant breakthrough. “Prior to this, we had no straightforward option to offer families of children who were becoming increasingly myopic. Now we have an effective treatment that has few side effects and works for most children,” he said.
Expert advice on usage. Currently, acceptance of this treatment in the United States has lagged behind Asia. Notably, data are lacking on how ophthalmologists should determine which children to treat,9 and no formal treatment guidelines are available. So what advice do the experts have for ophthalmologists who are interested in using low-dose atropine to treat their pediatric patients with myopia?
Adoption in the United States
Dr. Epley said that he sees the use of low-dose atropine becoming more mainstream. “Many colleagues are now using it, as compared to very few a year ago. As more ophthalmologists learn of the treatment’s benefits and risks, and as they see the study results, it is increasing in popularity.”
Ophthalmologists’ concerns. R. Michael Siatkowski, MD, at the Dean McGee Eye Institute in Oklahoma, noted that some U.S. pediatric ophthalmologists still do not use low-dose atropine. He suggested that some of them may be holding out for longer-term data on this approach—in particular because they are not yet convinced about the generalizability of the data from the ATOM studies to children with myopia in the United States. The ATOM studies were performed in Asia in a population of children with myopia who may differ substantially from those in the United States in terms of eye color, range of refractive error, study and recreation habits, and family history. And, even though results from the ATOM studies have been published in the medical literature, Dr. Siatkowski thinks they haven’t received enough coverage, for example, at local or regional medical meetings or in webinars.
Parental concerns. Like some ophthalmologists, some parents won’t try low-dose atropine until longer-term data are available, said Dr. Siatkowski. In addition, he said, “Some parents want to talk to other parents whose children have been treated with it, and others just don’t feel that their child will comply with the treatment regimen on a long-term basis. It does take some motivation on the part of the parents and kids to apply the drops daily.”
Another issue for some parents (and some ophthalmologists), he added, is that while low-dose atropine slows the progression of myopia, it doesn’t fully arrest it. For example, if a child has –2.0 D of myopia that could potentially increase to –3.0 or –4.0 D, some parents might consider the medication unnecessary because they don’t think there’s a big difference between these refractive errors, especially because the child will need glasses in either case, and the difference in uncorrected acuity may be comparatively small. However, “parents feel differently about a child with –4.0 D of myopia who could potentially increase to –8.0 D,” he said.
Longer clinic visit. From a clinician’s perspective, there may be concerns about patient flow. Although consultation time for patients with myopia tends to be relatively short, adding a discussion about atropine lengthens the visit, said Dr. Epley—especially since the use of a compounding pharmacy must be included. “But it’s the right thing to do for my patients, so I make the time.” Dr. Siatkowski noted that the discussion probably adds about 10 minutes to a routine consultation, and less when parents are already well armed with all the facts.
Off-label use. Because 0.01% atropine is not approved by the U.S. Food and Drug Administration for myopia, ophthalmologists need to discuss its off-label use with parents. However, according to Dr. Epley, “most families are accepting of this.” It also helps to have a compounding pharmacy to refer them to, he said. His office uses a local compounding pharmacy that charges $70 for a 10-mL bottle—about a 3-month supply. “If a family is from far away, I refer them to their local pharmacy for recommendations on a nearby compounding pharmacy.” Alternatively, he said, Leiter’s Compounding Pharmacy10 will ship the drug anywhere in the United States.
Although Dr. Siatkowski noted that he typically obtains 0.01% atropine for between $55 and $85 for a month’s supply, he said that cost rarely prevents parents from choosing the medication.
Minimal Side Effects
Ocular. Low-dose atropine has minimal effects on pupil size, accommodation, and near vision. “The average pupillary dilation in the ATOM2 study was 1 mm,” Prof. Tan said, noting that most patients receiving low-dose atropine have no need for bifocal eyeglasses or sunglasses. In addition, 0.01% atropine results in “minimal loss of accommodation of only about 4.0 D,” he said.
Pupil size. Because the ATOM study enrolled only Asian children, U.S. ophthalmologists may have concerns about the drug’s side effects in other patient populations. In Dr. Epley’s experience, atropine appears to be well tolerated by patients with lightly pigmented irides.
“In my clinical practice, there is mild pupillary dilation—2 mm or less among patients with blue eyes, and less than 1 mm in those with brown eyes. It’s rare for a Caucasian with blue irides to stop the drops due to near blur, as the drops cause no noticeable problem for the vast majority of patients.” The amount of pupillary dilation among patients with green or hazel eyes probably falls somewhere between the levels seen in those with brown and blue eyes, he said.
Systemic. Prof. Tan added that ophthalmologists may also be concerned about systemic side effects associated with atropine use.
Acute side effects. Although there is always a risk for systemic side effects with any medication, these appear to be rare with 0.01% atropine use, Dr. Epley said. “Tachycardia, altered mental status, dry mouth, urinary retention, constipation, and flushing skin have all been reported with higher doses of atropine—but not in any of the children in studies using low-dose atropine.”
Late side effects. With respect to potential late, long-term side effects, he noted that allergy would be the most likely to arise. While some ATOM2 participants experienced allergy-associated dermatitis (<1%) or allergic conjunctivitis (3%), no allergic reactions occurred in patients in the 0.01% group.4 “It’s possible that any of the known side effects of atropine could occur in the long term,” Dr. Epley added, “but the 5-year follow-up for ATOM2 did not report any children dropping out of the study for these reasons.”
In his own practice, Dr. Epley has about 120 children on low-dose atropine. Of these, he said, “I have 1 patient who developed allergy.” He noted that if an allergy to atropine develops, the drug must be discontinued. “Usually, that is the only treatment necessary if allergy develops.”
Potential Biomarker for Pathological Myopia in Adulthood?
In a recent retrospective study, researchers aimed to identify indicators for the development of pathological myopia in adulthood.1 Their study included 56 eyes of 29 patients with high myopia who were 15 years or younger at the initial visit and who were followed up at least once- yearly for 20 years. Two retina specialists compared fundus photographs obtained for each patient at both the first and last visit. They examined the images for evidence of pathological myopia, which was defined by high myopia and the presence of stage 2 or higher myopic maculopathy.
The results showed that 83% of the eyes of adults who developed pathological myopia had already shown evidence of diffuse chorioretinal atrophy during childhood. And although the diffuse atrophy was typically restricted to the temporal peripapillary area during childhood, it had expanded to cover the entire posterior fundus by adulthood.
Although the researchers acknowledged the limitations of their study, including its retrospective nature, as well as its small population size from a single center, they concluded that the presence of peripapillary diffuse chorioretinal atrophy in children with high axial myopia may be a biomarker for development of advanced chorioretinal atrophy in adulthood.
___________________________
1 Yokoi T et al. Ophthalmology. 2016;123(8):1783-1787.
|
Treatment Advice
Whom and when to treat. Prof. Tan uses 0.01% atropine in children from 6 to 12 years of age “who are at least –0.5 D myopic, and with a definite history of progression over the last few months—usually at least 0.5 D over the last 6 months.” Although the medication hasn’t yet been tested in children over 12 years of age, he added that it would not be unreasonable to use it in teenagers if their myopia is still progressing.
Similarly, Dr. Epley recommends low-dose atropine for children from 5 to 15 years of age. “Younger children are more likely to become more myopic over time than older children are, so they are of greatest concern.” He particularly recommends atropine for a child whose myopia is rapidly increasing. “I discuss this with any patient, or family of a patient, who has more than –1.0 D of myopia or who is increasing more than 1.0 D in a year,” he said.
Dr. Siatkowski follows a similar rule of thumb for starting the treatment: “Certainly, 1.0 D per year progression would be a red flag for me.”
Very young children. Both Drs. Epley and Siatkowksi said that axial myopia is rare in children under 5 years of age. “It’s not clear that children in this very young age group have the same mechanism for myopia as occurs in older children,” Dr. Epley said, “so I’m not currently treating the very young with atropine.” Dr. Siatkowski agreed and added that a refractive error of –1.0 D or more in a child under 5 years of age would be atypical and concerning, and it would lead him to first rule out other etiologies (such as anterior segment congenital malformation). Prof. Tan noted that a new trial will soon evaluate low-dose atropine in young children. “We intend to test it in children as young as 5 years of age who have progressive myopia,” he said.
How to treat. The treatment regimen requires patients or parents to administer 1 drop of 0.01% atropine, daily, in each eye. However, Drs. Epley and Siatkowski both agreed that the time of administration is not very important. Nighttime administration was traditionally the standard with higher doses of the drug because the side effects of the medication (pupillary dilation, reduction of accommodation) are less bothersome while the patient is asleep. However, Dr. Siatkowski stressed that this may not work well for some families. “Some do better remembering to administer it in the morning, or when they see it in their lunch box,” he said.
Duration of treatment. According to Prof. Tan, “it would seem prudent that we should use atropine for at least 6 months to see if it is working, and if it is having good results—i.e., myopia progression is lessening—then continue for at least 1 year in total in the first instance. One could then stop treatment and, if myopia starts up again, restart for another 6 months or a year.”
Dr. Epley uses 0.01% atropine to treat myopia in children either for 2 years or to 15 years of age, whichever is longer. “If a child’s myopia increases when we stop the atropine, I place them back on it for a year at a time until the eye has stopped growing.” He added that treatment has little effect on the child’s quality of life, “aside from the challenges of administering eye drops to children, who generally don’t like water in their eyes.” And Dr. Siatkowski tells parents to be prepared for their children to continue using the medication until they are 18 years old, and then wean off it—or to stop it sooner if they experience any problems.
What to expect. “In the first 6 months, the myopia may still progress—a finding that was also seen in the ATOM2 study,” Dr. Epley said. “After 6 months, the progression should slow significantly to –0.50 D change, or less, per year,” he added. According to Dr. Siatkowski, low-dose atropine has slowed the rate of myopic progression in his patients by between 30% and 50%. And 2 patients have had complete arrest of their myopic progression. “Both of these are Asian children with dark eyes who were moderate myopes to begin with,” he noted.
Follow-up during treatment. After starting a child on low-dose atropine, Prof. Tan stressed that follow-up after 6 months is the earliest time at which to begin assessing treatment efficacy. However, he typically evaluates children 3 months after treatment starts, to ensure they have no significant side effects. “It seems sensible to review every 6 months, thereafter, with cycloplegic refraction,” he said.
Dr. Epley said that he follows children “every 6 months while on the medication, to ensure compliance, to look for side effects, and to verify that the medication is working.”
Dr. Siatkowski typically follows up every 6 to 12 months (or sooner if the patient is having problems), depending on the child’s refractive error, as well as how quickly their myopia progresses. “If they’ve been progressing 1.0 D or more in a year, follow-up in 6 months would let me know whether the treatment has slowed it down,” he said. “But if their progression has been slower—say 0.5 D per year—I might wait 1 year to follow up.”
Follow-up after stopping treatment. When a child stops treatment, “the initial follow-up is at 6 months, then again at 12 months,” Dr. Epley said. “If there is no change in this period, then the child follows up in 1 year. If the child changes, we restart the drops and recheck in 6 months.” Thus far, in his practice, the only kids whose myopia began to increase rapidly after discontinuing atropine are those who stopped before completing at least 2 years of treatment.
More Data Needed
Dr. Siatkowski emphasized that some questions, inevitably, remain unanswered. As data continue to emerge, it may become evident that the optimum duration of treatment with low-dose atropine might depend on “factors such as the age when the drops were started, the starting refractive error, the rate of myopic progression, and parental refractive error history. It would also be good to have a registry to help answer these questions,” he said.
___________________________
1 Holden et al. Ophthalmology. 2016;123(5):1036-1042.
2 https://nei.nih.gov/eyedata/myopia/tables.
3 Chua W-H et al. Ophthalmology. 2006;113(12):2285-2291.
4 Tong L et al. Ophthalmology. 2009;116(5):572-579.
5 Chia A et al. Ophthalmology. 2012;119(2):347-354.
6 Chia A et al. Am J Ophthalmol. 2014;157(2):451-457.
7 Chia A et al. Ophthalmology. 2016;123(2):391-399.
8 Clark TY et al. J Ocular Pharmacol Ther. 2015;31(9):541-545.
9 Morgan IG et al. Ophthalmology. 2016;123(2):232-233.
10 Leiter’s Compounding Pharmacy. Available at https://leiterrx.com. Accessed Sept. 6, 2016.
___________________________
Dr. Epley is the owner of Children’s Eye Care, PLLC, in Kirkland, Wash. Relevant financial disclosures: Abbott Labs: O; Nevakar: C.
Dr. Siatkowski is David W. Parke II, MD Endowed Professor, Dean McGee Eye Institute, University of Oklahoma College of Medicine, Oklahoma City, Okla. Relevant financial disclosures: National Eye Institute: S.
Prof. Tan is Arthur Lim Professor, Ophthalmology and Visual Sciences Academic Clinical Program, Duke-National University of Singapore Medical School, senior consultant, Singapore National Eye Centre. Relevant financial disclosures: Alcon: S; Bausch & Lomb: S; Carl Zeiss Meditec: S; Network Medical Products: P; Santen: S.
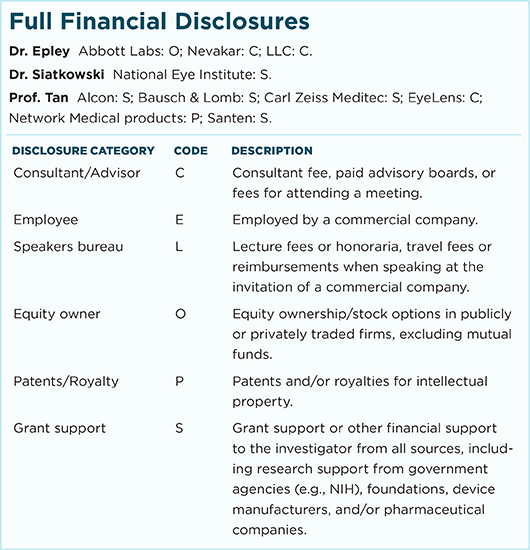
For full disclosures and the disclosure key, see below.