By Annie Stuart, Contributing Writer, interviewing Zélia M. Corrêa, MD, PhD, Prithvi Mruthyunjaya, MD, MHS, and Michael E. Snyder, MD
Download PDF
Primary iris cysts originate in the iris pigment epithelium or iris stroma, and secondary iris cysts are stimulated by outside factors. Most of these cysts are quite rare, but some can cause visual problems, requiring treatment. In addition, differential diagnosis is crucial to rule out more serious problems, mainly malignancies.1
Types of Iris Cysts
Although iris cysts are relatively rare, the following are more commonly seen.
Iris pigment epithelium cysts. The most common type of iris cyst, iris pigment epithelium cysts tend to show up on routine examinations because they are asymptomatic and rarely cause visual problems, said Prithvi Mruthyunjaya, MD, MHS, at Stanford University in Palo Alto, California. Although these cysts are typically referred to the ocular oncologist as a single iris mass of unknown origin, he said, they are often multifocal and bilateral.
Located underneath the iris, these cysts push the iris forward, creating a dome-shaped surface, said Zélia M. Corrêa, MD, PhD, at the University of Cincinnati. They may be midzonal, right in the middle of the iris leaflet, but also can be located at the inner or outer edges of the iris, near the pupil or ciliary body, potentially making them a diagnostic challenge. In some cases, these cysts may also detach from the iris and float freely in the anterior chamber or vitreous. They are translucent with speckles of light brown and are usually benign, said Dr. Mruthyunjaya.
Stromal cysts. Arising from the front part of the iris, stromal cysts tend to be translucent-white and can more readily deform the structure of the iris itself than iris pigment epithelium cysts do, said Dr. Mruthyunjaya. “This cyst can be confused for an iris melanoma, especially if it is strongly pigmented, making it look like a nodule.”
Epithelial downgrowth cysts. Following trauma—from either surgery or injury—epithelial cells may be transmitted from the outside of the eye to the inside, or cells inside the eye may transdifferentiate into epithelial cells, said Michael E. Snyder, MD, at Cincinnati Eye Institute.
“When surface epithelial cells get inside the eye, they do not behave nicely,” he said. “If they start forming an iris cyst, they are unlikely to cause immediate sight-impairing complications as long as they remain encased. But if they break or start growing into important structures of the eye, they can, rarely, cause fairly profound vision loss and sometimes loss of the eyeball itself.” In children younger than age 10, he added, these cysts can cover the pupil space, leading to amblyopia.
Because they grow toward the inside of the eye, Dr. Corrêa prefers to call them epithelial ingrowth—rather than downgrowth—cysts. “Although they may start developing years after the initial trauma,” she said, “they are very aggressive and can grow quickly, almost like a tumor, acquiring a surprising size.” Another interesting feature of these cysts, said Dr. Mruthyunjaya, is the proteinaceous reflectivity of the cystic fluid—they are not completely clear.
Confirming a Cyst Diagnosis
“I want to be able to properly identify the location and origins of a cyst,” said Dr. Mruthyunjaya. “That will involve a thorough history; complete examination, including a gonioscopy and examination of the anterior segment; and imaging. Sometimes looking at both eyes also provides clues about the etiology of the cyst.”
In the case of a suspected downgrowth cyst, he added, confirming etiology might also involve looking for surgical wounds or previous operative notes.
Don’t overlook history. “Curious and peculiar stories have underscored the importance of history-taking for me,” said Dr. Corrêa. She recounted the story of a civil engineer who felt “a slight snag” in his eye while overseeing the paving of a road. A tiny piece of gravel had lodged in his iris, but it didn’t raise red flags until months later when his vision became blurry from a developing cyst. Complicating matters, said Dr. Corrêa, the cyst looked like a tumor because the gravel was dark in color.
Dr. Snyder mentioned another instance in which history-taking is critical: Ask patients if they have traveled to other parts of the world where parasites are endemic; they may have experienced a parasitic infection. “Parasites that travel to the eye, such as Cysticercus cellulosae, can cause cysts that can be quite dangerous. If you inadvertently open the cyst and expose the parasite to the eye, it can die, causing a significant inflammatory response.”
Other questions to ask. Dr. Corrêa counsels colleagues to take time to talk with the patient and ask questions like these: How long have you been aware of the cyst? How long has it been since your last ophthalmology visit? What kind of exam did you receive? Did you have your pupils dilated?
If a cyst appears suddenly, said Dr. Mruthyunjaya, it’s worth asking whether the patient is on prostaglandin analogs, which can affect cyst size. Alert the doctor in charge of monitoring the eyedrops, especially if the cyst has become quite large.
Imaging. To rule out other problems and diagnose an iris cyst, ophthalmologists may use either anterior segment OCT or high-resolution ultrasound biomicroscopy (UBM), said Dr. Corrêa. “As long as you scan the whole cyst and have a good enough image of the lesion, you’re in great shape,” she said, adding that each diagnostic modality has its advantages.
Advantages of OCT. Anterior segment OCT may identify small cystic structures, giving early confirmation of diagnosis. However, it does have limitations. For example, in patients with dark irides, the OCT signal may become attenuated, said Dr. Mruthyunjaya. Also, the pigmentation or size of the cyst may prevent ideal resolution, he said. “But I’ve been impressed with the ability to penetrate even small cysts,” he said, adding that repeatedly scanning the same area also provides a useful way to follow up on a cyst’s growth over time. OCT also has the advantage of no contact with the patient’s eye, said Dr. Corrêa, which can be especially helpful for younger patients.
Although Dr. Mruthyunjaya finds OCT helpful in imaging peripheral cysts, Dr. Corrêa warned that it may not be possible to see the full extent of these cysts with OCT, especially if they are large.
Advantages of ultrasound. High-resolution ultrasound of the anterior segment provides a very good view, allowing you to visualize thin walls and hollow cavities, indicating a fluid-filled cyst, versus the solid nature of a malignancy, said Dr. Snyder. In addition to looking at the quadrant of the suspected cyst, Dr. Mruthyunjaya’s initial evaluation involves a scanning protocol around the peripheral part of the iris and ciliary body—as well as the other eye. “It’s striking how often you will find tiny cysts in multiple locations that weren’t detected clinically.”
Dr. Corrêa also uses UBM for surgical planning. “It’s easier to turn the probe around and get a feel for the extent of the cyst and consistency of the tissue.” Those who lack experience with UBM should consider referring this out, she said.
What’s next? If you see a lesion with a solid component, you might confirm this with magnetic resonance imaging, said Dr. Corrêa, and even biopsy for confirmation of malignancy.
When Cancer Is a Concern
“Although it is easier to assume that small lumps or bumps in the iris are benign,” said Dr. Corrêa, “in the back of your mind, you need to consider other more serious differential diagnoses. Always remember that tumors can be occasionally associated with cysts or have a cystic component.”
Most worrisome. In her practice, Dr. Corrêa has seen a number of iridociliary melanomas with a cystic component located right at the root of the iris. “I’ve also seen patients with medulloepithelioma, a rare type of neuroectodermal tumor that can be aggressive and have a prominent cystic component, especially ones in the ciliary body.” Most worrisome, she said, are tumors in the transition between the iris and ciliary body. They are usually hidden, harder to diagnose, and trickier to treat. “You must rely on imaging such as high-resolution ultrasound because it’s hard to visualize them directly or indirectly,” she said.
Other serious signs. “Any time you see an iris lesion associated with prominent episcleral blood vessels, unexplained acute increase in intraocular pressure, or iris heterochromia,” she said, “a neoplasm should be in the differential diagnosis.” Also, patients with localized graying or darkening of the sclera should be cautiously evaluated to rule out a melanocytic tumor, she said. Using transillumination, it is possible to identify a melanocytic lesion, which almost always will cast a dark shadow.
|
When Treatment Is Needed
In most cases, Dr. Corrêa simply observes iris pigment epithelial and stromal cysts.
Conditions dictate choices. However, said Dr. Corrêa, treatment may be needed if there are other problems such as increasing eye pressure or multiple cysts occluding the angle. Consider other conditions as well, said Dr. Mruthyunjaya: Is there an incomplete wound involved in epithelial downgrowth that you need to address? What is the size of the cyst and its velocity of growth? Is it intermittently leaking and causing inflammation? Is it rubbing against ocular structures such as the lens or the cornea, causing secondary problems?
Treat it like a tumor? Dr. Snyder said it is most effective to treat epithelial downgrowth cysts as though they are tumors, as they cause unrestricted growth of cells where they don’t belong. “Sometimes, treatment’s one and done,” said Dr. Mruthyunjaya, “but sometimes it requires multiple attempts at controlling the cyst. In other cases, reduction is good enough. Regardless, you need to watch them closely.”
What to consider beforehand. You can use a variety of options to treat epithelial downgrowth cysts. “But whatever you do with these cysts,” said Dr. Corrêa, “you must remove every little bit of abnormal epithelium from the anterior chamber, or the cyst may recur, proliferate rapidly, and cause a lot of damage inside the eye.” Before any procedure, ensure that imaging has revealed the full extent, size, and location of the cyst, she said, so you can approach it the right way.
Excision. To cause less collateral damage, Dr. Mruthyunjaya prefers excising these cysts when they are small. Dr. Snyder recommends a partial lamellar iridocorneal trabeculectomy—removing the internal eye wall and the areas the cyst is touching—to avoid rupturing or breaking the wall of the cyst. “If this procedure creates a serious iris defect,” he said, “it often causes glare or light sensitivity. If it is not possible to surgically close the area that’s been removed, an artificial iris may be needed.”
Drainage and injection. Dr. Corrêa also likes to treat ingrowth cysts by using a needle to drain the cyst, inject alcohol inside it, and then deflate the cyst. “In case there is any sign of residual epithelium on the surface of the iris, I use an endolaser probe to treat the area and make sure any epithelial cells are destroyed.”
To minimize the chances of leaving cells behind, Dr. Mruthyunjaya recommended avoiding going through the open aqueous humor and anterior chamber. “Try to go through the back or more peripheral part of the cyst. Consequently, if there’s anything that’s being released when you pull in and out of the eye, it’s coming right out of the eye with your needle.”
Dr. Mruthyunjaya also uses fluorescein eye stain to make sure the alcohol is contained within the cyst and not accidentally instilled into the anterior chamber, where it can be very toxic. Filling the eye with Healon viscoelastic also acts as a diffusion barrier for the alcohol, he said, but the viscoelastic must be thoroughly removed after the procedure.
Cryotherapy. Following drainage and injection, Dr. Mruthyunjaya then uses cryotherapy at the edge of the track by the limbus to sterilize any cells that may be remaining. Sometimes it is possible to freeze an entire cyst if it is tiny and located peripherally, right at the edge of the cornea at the limbus, added Dr. Snyder.
___________________________
1 Shields JA, Shields CL. Asia Pac J Ophthalmol. 2017;6(1):64-69.
___________________________
Dr. Corrêa is professor of ophthalmology at the University of Cincinnati in Ohio and director of the Ocular Oncology Program. Relevant financial disclosures: None.
Dr. Mruthyunjaya is associate professor of ophthalmology at Stanford University and director of ocular oncology at the Byers Eye Institute in Palo Alto, Calif. Relevant financial disclosures: None.
Dr. Snyder is chair of clinical research and on the board of directors at Cincinnati Eye Institute and is associate professor of ophthalmology–affiliated, at the University of Cincinnati in Ohio. Relevant financial disclosures: HumanOptics: C.
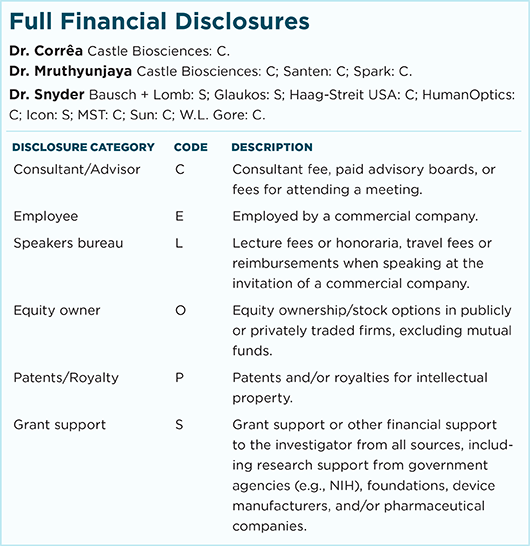
For full disclosures and the disclosure key, see below.