Download PDF
Ocular imaging is used extensively for making clinical decisions in ophthalmology. In fact, efficient patient care has increasingly become dependent on the rapid retrieval of this data. As in other specialties, systems that provide convenient retrieval of imaging data are becoming an integral part of many ophthalmic practices. However, before you invest in an image management system, it is important that you do some groundwork.
Assess the Advantages
Why should you consider investing in an image management system?
Improved access to images. “Almost all ophthalmic imaging devices generate digital data. The next logical step is viewing it digitally,” said Michael F. Chiang, MD, of the Oregon Health & Science University. “One of the greatest benefits of this advance is that we can now retrieve patients’ images in real time. Once an image is generated, it can be viewed immediately. Images can be viewed remotely or sent out for second opinions.”
Easier to compare images. The ability to compare images electronically from multiple patient visits is another significant advantage. “I can review a patient’s last four OCT images on one screen, for example, which makes my clinical decisions more proficient,” said Jeffrey L. Marx, MD, at the Lahey Clinic in Burlington, Mass. “In the past, the paper chart was disassembled, and hard copy images were spread out on a desk in order to visualize and assess changes between visits—a process that was inefficient and cumbersome.”
Help in analyzing images. Some systems include software that makes it easier to assess pathologies. “Processing methods can enhance an image or highlight certain features,” said Dr. Chiang. “And in some cases, investigators have developed algorithms to assist with clinical diagnoses or to determine whether a patient’s findings are getting better or worse.”
Patient data can be more secure. Compared with paper records, electronic archiving can be a much more secure way of storing and handling data, said Jeffery Daigrepont, a consultant whose firm, the Coker Group, participates in the AAOE’s Consultant Directory. “Auditing logs record every time an image is accessed. And all modifications are documented by date, time, and employee.”
Infrastructure?
“The major catalyst for failure in an implementation project [e.g., deploying an image management system] is poor network infrastructure,” said Kyle Chang, who manages IT services at a consultancy. “You can buy a top-notch system, but if it is paired with a switch or router from your local office supply store, the network will be quickly overwhelmed by the substantial requirements of an imaging system—or any other large-scale database.”
A system is only as good as the network it is running on. “One of my primary tasks last year was reviewing clients’ network capacity, hard drive space, and databases to make sure they were running at optimal performance levels. Nine times out of 10, they were not,” said Mr. Chang.
How much storage space do you need? “We typically see 10 to 12 gigabytes of growth per provider, per year. This is in addition to scanning the existing images into the system,” said Mr. Chang who helps clients estimate their storage requirements.
|
Before You Buy: Considerations
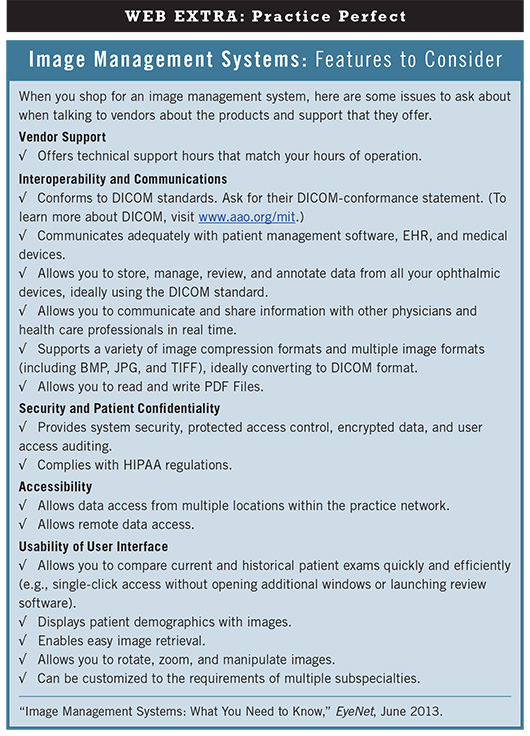
Know your goals. “First and foremost, a practice should contemplate what it wants to accomplish with an image management system,” said consultant Jeff Grant. Some EHR systems have built-in image management capabilities that might be suitable for a smaller practice’s needs. Conversely, multilocation, multispecialty practices with numerous devices will likely require a system that is more robust. “Regardless of your practice size, think about what functionality you might want,” said Mr. Grant. “For instance, do you want the ability to access images remotely? Do you want a system that manages all of your digital equipment output? Do you want to compare and manipulate images? After establishing a list of requirements, talk to your vendor and ask what infrastructure you will need to make the system work effectively.”
DICOM compliance is essential. Until recently, most image management systems interacted with imaging devices via proprietary interfaces and did not rely on the Digital Imaging and Communications in Medicine (DICOM) standards (www.aao.org/mit). However, “during the last decade, the Academy has helped develop DICOM standards for all of ophthalmology’s major testing modalities, and there has been significant movement toward standards-based imaging in our specialty by vendors over the last two years,” said Michael V. Boland, MD, PhD, of the Wilmer Eye Institute.
“When selecting a new system, consider only those that are DICOM compatible, request a copy of the vendor’s DICOM compliance statement, and review it to ensure the system will cohesively integrate with your existing hardware, software, and devices. This will eliminate the need for developing proprietary interfaces,” said Dr. Boland.
Don’t skimp on disk storage space. “Do not underestimate the amount of space you will need for storing images. When a vendor suggests using a certain amount of storage space, double or even triple it,” said Dr. Marx. “Image data increases exponentially, so you may need to install additional storage space to accommodate your growing database at some point. Even if you need hundreds of gigabytes, or a terabyte or more, there are devices that can handle these large volumes at reasonable prices,” said Mr. Grant.
Evaluate workflow to determine database design. “The key to imaging, from an operational standpoint, is how the images are archived and indexed within the database,” said Mr. Daigrepont. “For example, when consulting with a repeat patient, you typically want diagnostic images saved in reverse chronological order so you can look at the most recent one first and the oldest one last—much as you would with a paper chart. Think about the natural workflow of each physician in your practice and construct the digital system to mimic this routine.”
Observe the technology in action. Visit practices that already have a system in place in order to see how it works. “Although it is always helpful to see a vendor’s demonstration, the people conducting the presentation are usually the product creators, or they are very well trained,” said Dr. Marx. “It is quite different, however, once you install a system and only then realize that it takes 20 clicks to reach the functions necessary to access data and make a clinical decision. It is vital to see how the technology works in a real-world scenario first to avoid potential regrets.”
Know when (and when not to) upgrade. “If you are already using an image management system and are considering an upgrade, now is the perfect opportunity to address any performance or functionality issues with your current vendor,” said Mr. Daigrepont. “Equally important, never assume that an upgrade is going to be a better version of what you already have in place. Even though it is the same basic product, revised programming could adversely affect your functionality.” If you decide to upgrade your image management system, you should create a test environment on your network and try the upgrade on that before you completely remove the old system, said Mr. Daigrepont. “We also urge clients to resist being the first to test an upgrade until it has been in use for a while so the vendor has time to resolve any inherent problems.”
More Emphasis on Functionality
“In the past, the focus has been on connectivity issues,” said Dr. Marx. “Moving forward, connectivity will be assumed and the emphasis will be on functionality—the ability to present the data obtained from imaging devices in a simple way so that we can make clinical decisions. For example, when we measure a retinal thickness of 400 micrometers with an OCT and then send the image to our image management system, it is stored as a PDF file. The actual measurement, however, does not become a part of the file unless I enter an annotation. Now that we are focusing more on functionality, we want the system to be able to extract the data embedded within these images in such a way that it can be compared to previous images and analyzed for changes. The technology is in its infancy now, but vendors are working toward these capabilities.”
Michael V. Boland, MD, PhD, is a member of the Academy Medical Information Technology MIT Committee and is assistant professor of ophthalmology and director of information technology at the Wilmer Eye Institute. Financial disclosure: Is a consultant for Allergan and Carl Zeiss Meditec. Kyle Chang is senior manager of IT services at the Coker Group, a nationwide consultancy firm headquartered in Atlanta. Financial disclosure: Is employed by a consulting firm. Michael F. Chiang chairs the Academy MIT Committee and is professor of ophthalmology, medical informatics, and clinical epidemiology at Oregon Health & Science University, Portland. Financial disclosure: Is an unpaid member of the scientific advisory board for Clarity Medical Systems. Jeffery Daigrepont is senior vice president at the Coker Group. Financial disclosure: Is employed by a consulting firm. Jeff Grant is president of HealthCare Management & Automation Systems, a Wyoming-based consultancy firm. Financial disclosure: Is employed by a consulting firm. Jeffrey L. Marx, MD, is chairman of ophthalmology at Lahey Clinic and associate clinical professor of ophthalmology at Tufts University School of Medicine. Financial disclosure: No related financial interests.