By Linda Roach, Contributing Writer, interviewing Emmett T. Cunningham Jr, MD, PhD, MPH, and Pravin U. Dugel, MD; and reporting from the 2015 OIS, AAO, and Retina Subspecialty Day
Download PDF
After nearly a decade of treating retinal diseases with anti-VEGF drugs, ophthalmologists are well aware of the limitations of this therapeutic approach. So it is good news indeed that dozens of novel compounds—and innovative ways to deliver them—are being investigated for signs that they might make existing retinal drug therapies more effective and reduce the frequency of intravitreal injections.
The November 2015 Ophthalmology Innovation Summit (OIS) and Retina Subspecialty Day, both held in conjunction with AAO 2015, provided an overview of numerous retinal drugs in the development pipeline. Following are some highlights from those meetings, along with additional perspective from Emmett T. Cunningham Jr, MD, PhD, MPH, and Pravin U. Dugel, MD.
There is a particular need for new treatment protocols that would reduce the burden of anti-VEGF injections in patients with neovascular age-related macular degeneration (AMD), said Dr. Cunningham. He is an ophthalmologist and a venture capitalist who founded and cochairs the OIS.
Despite a strong and direct correlation between the total number of anti-VEGF injections per year and better visual outcomes,1 patients and their caregivers often have difficulty meeting the recommended, per protocol dosing frequency, Dr. Cunningham said. One study of drug usage patterns in the United States found that AMD patients treated with bevacizumab and ranibizumab received an annual average of only 5.3 and 6.8 injections, respectively.2 These numbers are even lower outside of the United States.
“Basically, treating physicians are giving half as many injections as the study protocols showed to be effective, and we know that fewer injections are less effective. So I think compliance is going to emerge as a very important metric” when evaluating new AMD drugs, Dr. Cunningham said.
Drug Combinations
Pegpleranib (Fovista) is further along the road toward possible clinical use than other investigational AMD drugs. Pegpleranib is a peptide aptamer that inhibits the activity of platelet-derived growth factor (PDGF), which plays an important role in the establishment and growth of choroidal neovascularization.
Good early outcomes. In the phase 2b trial, patients who received intravitreal pegpleranib (1.5 mg) concurrently with ranibizumab gained a mean of 10.6 letters in visual acuity at 24 weeks, compared with 6.5 letters in the ranibizumab monotherapy group (p = .019). Two large phase 3 clinical trials of combined pegpleranib and ranibizumab are under way, and a third phase 3 trial is planned to test the drug’s effectiveness when combined with bevacizumab or aflibercept, Ophthotech says.3 The company expects to have 12-month clinical outcomes from the first 2 phase 3 clinical trials late in 2016.
A 2-pronged molecular attack. Retina subspecialists are eagerly awaiting the addition of a PDGF inhibitor like pegpleranib to their clinical armamentarium because targeting a second molecular pathway makes biological sense, said Dr. Dugel, managing partner of Retinal Consultants of Arizona, in Phoenix. “With anti-VEGF alone, we’ve reached a ceiling in terms of therapeutic effect. One reason for this is that every anti-VEGF injection that you give upregulates PDGF,” he said. “PDGF recruits mature pericytes to cover the neovascular complex. So, in effect, by repeatedly giving VEGF-inhibitor monotherapy, you’re making the membrane more resistant to further anti-VEGF treatment.”
Greater benefit with pretreatment? Dr. Dugel performed a small 24-month, independent, open-label antifibrosis study that examined the utility of pretreatment in a randomized group of patients, the majority of whom were treatment resistant. (The mean number of injections prior to enrollment was 25, and 89% of participants had a treatment frequency of 6 weeks or less.) He presented his results at Retina Subspecialty Day.
He injected 10 patients intravitreally with pegpleranib the day before giving them a second pegpleranib dose plus a VEGF inhibitor. The 17 control eyes received both drugs on the same day, about 30 minutes apart. (After 3 loading doses, subsequent injections were given on an as-needed basis.) After 18 months, the pretreated patients showed a mean gain of 20 letters of visual acuity, compared with a 2-letter gain in the simultaneous-injection group, Dr. Dugel reported.
If an ongoing company-sponsored study (expected to end in May 2017) confirms his results, this would call into question the rationale and the utility of having a coformulated or a biphasic drug, Dr. Dugel said. “Do you really want to have both drugs in 1 vial if pretreatment actually shows a better effect? It may be better to have the 2 uncoupled, so you can pretreat and have the opportunity to choose the anti-VEGF.”
Sustained-Release Drugs
GB-102 (GrayBug). This sustained-release product contains a small-molecule compound, already FDA approved for treating cancer, that inhibits both VEGF and PDGF activity. The drug is incorporated into a proprietary biodegradable carrier system: polymer microparticles that release the drug over a 4- to 6-month period, Jeffrey L. Cleland, PhD, GrayBug’s interim CEO, said at the OIS meeting. The drug-carrying particles are injected into the vitreous with a 27- to 29-gauge needle, he said.
In rabbit studies so far, GB-102 delivered intraocular medication for at least 3 months, with no inflammation or toxicity, Dr. Cleland said. The company expects to begin FDA clinical trials of GB-102 this year.
NT-503 in Encapsulated Cell Technology (ECT; Neurotech). Part drug and part device, NT-503 is a novel VEGF receptor protein, produced by recombinant retinal pigment epithelial (RPE) cells encapsulated in a semipermeable membrane. The physician inserts the implant into the back of the eye through a 3-mm scleral incision.
Neurotech hopes that the RPE cells will produce the receptor-blocking protein in patients’ eyes for as long as 2 years, a claim that is currently being tested in a 150-patient phase 2 clinical trial. The trial is comparing NT-503 to aflibercept for recurrent neovascularization from AMD. Initial results from the trial are expected in late 2017.
AR-13154 (Aerie Pharmaceuticals and GrayBug). In addition to targeting PDGF, AR-13154 acts against 2 other intracellular signaling molecules involved in retinal neovascularization: Rho kinase (ROCK) and Janus kinase 2 (JAK2). A preclinical study in rats found that AR-13154 reduced the size of choroidal neovascular lesions more than did aflibercept, Aerie CEO Vince Anido Jr, PhD, reported at the OIS meeting. Last year, Aerie entered a partnership with GrayBug to encase AR-13154 in the latter company’s sustained-release polymer microparticles.
New Routes to the Retina
Self-injection: AKB-9778 (Aerpio Therapeutics). This first-in-class small molecule is being investigated as a systemic treatment for diabetic macular edema (DME) in combination with intravitreal ranibizumab. Diabetic patients would self-administer AKB-9778 daily by subcutaneous injection.
The drug inhibits an enzyme, human protein tyrosine phosphatase β, that downregulates the Tie2 receptor in retinal cells. In a 144-patient proof-of-concept clinical trial, the resulting restoration of Tie2 signaling alleviated vascular destabilization and reduced macular edema compared with ranibizumab-only eyes (p = .02), according to Peter A. Campochiaro, MD, who spoke at Retina Subspecialty Day. (Dr. Campochiaro is a consultant to and receives grant support from Aerpio.)
Furthermore, the twice-daily subcutaneous injections (15 mg) of AKB-9778 improved the subjects’ scores on the diabetic retinopathy severity scale by 2 or more steps—even if they did not have DME—Dr. Campochiaro said. Consequently, Aerpio officials say they are considering formal clinical trials to evaluate the drug as a treatment for diabetic retinopathy itself.4
Oral: X-82 (Tyrogenex). This inhibitor of both VEGF and PDGF is being investigated as a way to reduce the frequency of existing AMD treatments—without requiring any additional intravitreal injections. Instead, X-82 comes in tablets that patients would take daily.
Tyrogenex reported that patients in a phase 1 safety study (NCT01674569), which combined X-82 with as-needed (rescue) ranibizumab, had stable or improved visual acuity during the trial. Most did not require any injections.5 Results are expected late this year from a placebo-controlled phase 2 study (NCT02348359), which is combining X-82 therapy with as-needed aflibercept.
Topical: PAN-90806 (PanOptica). At OIS, Paul Chaney, CEO of PanOptica, said that if PAN-90806 shows effectiveness in clinical trials, this selective VEGF-receptor antagonist—delivered in eyedrops—could be a game-changer in the treatment of wet AMD and proliferative diabetic retinopathy.
Animal studies suggest that PAN-90806 penetrates well to the choroid and retina and can persist for as long as 17 hours, he said. Adverse events in a phase 1 safety/dosing study, which ended in late 2015, were limited to reversible ocular surface problems at higher dosage levels, he added.
The second stage of the trial is dosing 10 AMD patients with an initial ranibizumab injection, followed by up to 12 weeks of daily PAN-90806 eyedrops. Mr. Chaney reported that, as of November, 4 people had completed the 12-week regimen, and none had required a rescue intravitreal injection. Final results will be available in early 2016, he said.
Retina Subspecialty Day
Be sure to check out AAO Meetings on Demand for cutting-edge information presented during the Retina Subspecialty Day sessions. AAO Meetings on Demand does not provide CME credit.
To order, visit www.aao.org/ondemand.
|
Gene Therapy
SPK-RPE65 (Spark Therapeutics). The eye is the site where researchers completed the first randomized controlled phase 3 clinical trial demonstrating long-lasting gene replacement in any inherited human disease. Patients with Leber congenital amaurosis (LCA) regained functional low-light vision after a single subretinal injection with a recombinant adeno-associated virus.
Jeffrey D. Marrazzo, Spark’s CEO and cofounder, said at OIS that the company expects to submit the recombinant viral vector to the FDA for therapeutic approval in 2016.
Other retinal gene therapy efforts are in development, Dr. Cunningham said. “We now have 1 positive phase 3 gene therapy trial, but people want to see if it translates into multiple indications, some of which have underlying anatomic changes associated with the gene defects that may or may not limit therapeutic benefit,” he said.
Applied Genetic Technologies is conducting a small safety/dosing clinical trial of an adeno-associated viral vector, rAAV-hRS1, to treat X-linked retinoschisis. The recombinant virus carries a gene for retinoschisin, the structural protein missing in affected patients. A report on the early outcomes is expected in December 2016, with the final phase 2 analysis complete in late 2020.
Meanwhile, the company will use the same vector design strategy in 2016 and 2017 to investigate gene therapy for different forms of achromatopsia, the company’s chief scientific officer, Mark S. Shearman, MD, PhD, said at OIS. He added that the company also plans to pursue gene replacement for X-linked retinitis pigmentosa.
Avalanche Biotechnologies has a pipeline of viral vectors—all in early clinical testing phases—that are intended to inhibit VEGF or to replace missing proteins in retinal diseases. The targets so far include wet AMD, X-linked retinoschisis, and red-green color blindness. The vector that is furthest along in clinical testing is AVA-101 (also called rAAV.sFlt-1). The sFlt-1 protein inhibits angiogenesis and reduces vascular permeability.
___________________________
1 Holekamp NM et al. Am J Ophthalmol. 2014;157(4):825-833.
2 Kiss S et al. Ophthalmic Surg Lasers Imaging Retina. 2014;45(4):285-291.
3 http://investors.ophthotech.com/releasedetail.cfm?ReleaseID=943051. Accessed Dec. 12, 2015.
4 www.aerpio.com/news/AAO-Data-Release.pdf. Accessed Dec. 12, 2015.
5 www.prnewswire.com/news-releases/tyrogenex-presents-final-results-from-phase-1-study-of-x-82-for-wet-amd-at-the-2015-annual-american-academy-of-ophthalmology-meeting-300178524.html.
___________________________
Dr. Cunningham specializes in infectious and inflammatory eye diseases at West Coast Retina Medical Group, San Francisco. He is director of the Uveitis Service at California Pacific Medical Center, San Francisco; adjunct clinical professor of ophthalmology at Stanford University School of Medicine, Stanford, Calif.; and a research associate at the Francis I. Proctor Foundation for Research in Ophthalmology, at UCSF School of Medicine. He is also a partner in Clarus Ventures and is founder and cochairman of the Ophthalmology Innovation Summit. Relevant financial disclosures: None.
Dr. Dugel is a retina subspecialist and managing partner of Retinal Consultants of Arizona, in Phoenix, and a clinical professor at the University of Southern California Eye Institute, in Los Angeles. Relevant financial disclosures: Abbott: C; Acucela: C; Alcon: C; Alimera: C,O; Allergan: C; Digisight: O; Genentech: C; Novartis: C; Ophthotech: C,O; Ora: C; Regeneron: C; ThromboGenics: C. NOTE: Biographical information and financial disclosures are not provided for corporate speakers at OIS, as their roles and proprietary interests are self-evident.
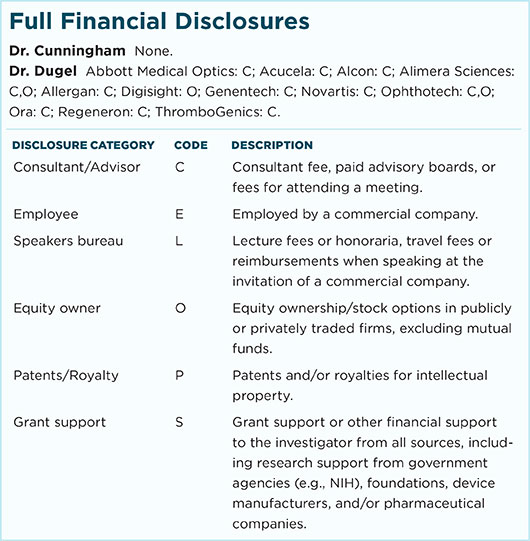
For full disclosures and the disclosure key, see below.