Intravitreal Bevacizumab or Laser for ROP: 4-Year Outcomes
By Lynda Seminara
Selected By: Stephen D. McLeod, MD
Journal Highlights
Ophthalmology, February 2018
Download PDF
As the survival rate for infants with very low birth weight has increased, so have concerns about improving long-term outcomes for retinopathy of prematurity (ROP). Laser ablation is still the standard of care for ROP, but anti–vascular endothelial growth factor (VEGF) drugs, including intravitreal bevacizumab, have generated interest. To compare long-term outcomes of ROP treatment, Lepore et al. conducted a follow-up study of infants born prematurely with type 1, zone 1 disease who had received bevacizumab or undergone laser photoablation. They found that serious ocular effects were more likely to remain in bevacizumab- treated eyes.
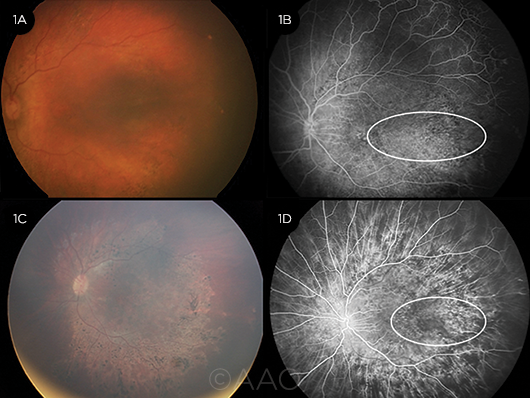 |
ROP. Color fundus (1A) and FA (1B) 9 months after bevacizumab injection, with an area of retinal capillary hypoperfusion evident (white circle). Four years later, significant pigmentary abnormalities are evident at the posterior pole (1C), as is a persistent lesion on FA (1D, white circle).
|
The authors’ randomized trial was conducted at Catholic University in Rome from September 2009 through March 2012. Twenty-one infants (42 eyes) received laser photoablation of the peripheral avascular retina in 1 eye and an injection of bevacizumab 0.5 mg in the other. Fluorescein angiography (FA) was performed before and 9 months after treatment. At an average of 4 years after treatment, additional digital retinal and FA images were obtained. Two ROP experts assessed images of 20 eyes in the bevacizumab group and 19 in the laser group for retinal and choroidal features.
At 4 years of age, abnormalities persisted in many bevacizumab-treated eyes, including vessel leakage (13 of 19 eyes), abnormal vessel branching (17 of 20 eyes), vascular tangles (15 of 18 eyes), and shunts (17 of 18 eyes). The authors attributed these problems to ongoing circulation issues. In contrast, fewer laser-treated eyes showed vessel leakage (1 of 18 eyes), abnormal shunts (2 of 19 eyes), or tangles (1 of 18 eyes). No branching abnormalities were observed in this group.
Moreover, at the posterior pole, hyperfluorescent lesions persisted in 55% of bevacizumab-treated eyes and 16% of laser-treated eyes.
The authors noted that many of these outcomes are “worrisome,” but they emphasized the importance of FA in identifying unresolved abnormalities. Modalities such as FA and optical coherence tomography could become instrumental in selecting eyes for treatment and determining the timing of interventions. The authors urged clinicians to consider systemic as well as ocular health in their efforts to optimize treatment for infants with serious ROP.
The original article can be found here.