Download PDF
A decade ago, at a meeting of WaveLight laser users, Theo Seiler, MD, PhD, presented early results on a procedure that he had developed for strengthening the cornea in patients with keratoconus. The procedure, corneal collagen cross-linking (CXL), was having a dramatic effect on keratoconus. By creating stronger collagen bonds, CXL made the cornea more rigid and appeared to halt disease progression.
But the postoperative refractive outcomes were less impressive, recalled David T. C. Lin, MD, who attended the meeting. “Patients were better, but we weren’t getting them close to good functional vision.”
Dr. Lin, who is clinical associate professor of ophthalmology at the University of British Columbia and medical director at Pacific Laser Eye Centre in Vancouver, Canada, spent the ensuing years developing a treatment that would deliver a one-two punch to both normalize the corneal topography and enhance visual acuity. His solution: CXL plus laser ablation.
At the same time, other researchers were exploring different combinations of procedures to achieve the same result. Combined treatment makes sense for a multifactorial disease like keratoconus, in which the clinical challenge is twofold: to stop disease progression and improve vision, said Peter S. Hersh, MD, director of the Cornea and Laser Eye Institute - Hersh Vision Group, as well as professor of clinical ophthalmology and director of the Cornea and Refractive Surgery Division, UMDNJ-New Jersey Medical School.
Most keratoconus combos include CXL plus something else, and there are many possible permutations. Yaron S. Rabinowitz, MD, director of ophthalmology research, Cedars Sinai Medical Center, and clinical professor of ophthalmology, University of California, Los Angeles, rattled off a list: CXL plus intracorneal ring segments (most commonly Intacs); CXL plus phakic intraocular lens (PIOL); CXL plus Intacs plus PIOL; CXL plus PRK; CXL plus Intacs plus PRK.
Although researchers have reported promising results with some of these combinations, there’s a catch. CXL is not FDA approved, although it received the CE mark more than five years ago. Moreover, some of the other procedures and devices may be approved for refractive use but not for keratoconus, although Intacs has received an FDA humanitarian device exemption for this indication. Patients in the United States can receive CXL monotherapy or combined treatment only by enrolling in a formal clinical trial or by traveling to countries where it is available. The good news: This is a highly active area of research, with more than 100 clinical trial sites throughout the United States currently offering CXL alone or in combination (see “Refer Your Patients to a Trial”). The bad news: Patients often have to pay out of pocket for the procedures.
|
Collagen Cross-Linking
|
 |
|
The interaction of UVA and riboflavin creates stronger collagen bonds in the cornea.
|
The Basic Procedures
At one end of the spectrum of keratoconus patients are those who are not progressing and have acceptable vision with contact lenses; at the other are those with severe disease who may have no option other than corneal transplant. In between are patients who are intolerant of or poorly corrected with lenses or those who are progressing but may not require—or wish to avoid—transplantation. The following procedures, used alone or in combination, may provide alternatives.
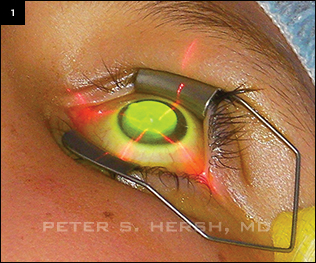
CXL. This treatment to stop progression of keratectasia involves the interaction of ultraviolet-A light (UVA) with the photosensitizer riboflavin (vitamin B2) to strengthen the chemical bonds between collagen fibrils in the cornea through oxidative reactions. A pilot study demonstrated a 328.9 percent increase in the rigidity of the human cornea using CXL in laboratory experiments.1
“CXL has as its primary purpose the stability of the cornea to prevent natural progression of corneal ectatic disease,” Dr. Hersh said. “On average, there is some improvement in topography and some improvement in vision.2 But the main role of CXL is to strengthen the biomechanics of the cornea to prevent progression.”
Intracorneal rings. Worldwide, several different types of intracorneal ring segments are used for refractive correction and treatment of keratoconus, but the only brand approved in the United States is Intacs (Addition Technology). The device consists of two clear, curved plastic segments, available in a range of thicknesses, which are implanted through a small surgical incision at the perimeter of the cornea to improve corneal topography in patients with keratoconus. Intacs work by flattening the cornea and improving corneal symmetry. They can be placed as symmetric segments of matching thickness or as asymmetric segments (generally a thicker segment inferior to the cone and a thinner segment above); in some cases, only a single segment is used. Refractive error and corneal topography are used to determine the appropriate segment thickness, combination, and positioning.
Intacs should not be used in patients whose keratometry readings exceed 58 D, said Dr. Rabinowitz, who also directs the Keratoconus Center, a research and treatment center in Beverly Hills. He uses the Intralase femtosecond laser to create the channels that hold the plastic segments. Other surgeons create the channels mechanically with metal blades.
Topography-guided photorefractive keratectomy (TG-PRK). Topography-guided excimer laser ablation was introduced more than 10 years ago to treat highly irregular corneas. Several companies have systems for TG-PRK, though none is yet approved in the United States. Treatment is generally limited to a 50-µm maximum tissue removal (for a residual stromal depth of at least 300 µm), guided by a corneal topography map. The map is created by multiple high-resolution computer images. This allows imaging of difficult corneas, even those with extreme cones or keratometry greater than 60 D. Treatment algorithms are then developed to flatten or steepen specific meridians as needed, based on a best-fit sphere.
 |
|
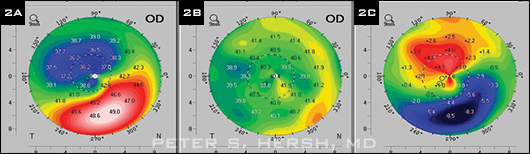
ACXL PLUS INTACS. (2) Corneal topography of patient who had CXL and Intacs. (A) Preoperative topography. (B) One year after CXL followed by placement of one 400-µm Intacs segment three months later, map shows improved symmetry of topography. (C) Difference map; note flattening of 8.5 D over cone apex.
|
A Menu of Possible Combinations
CXL plus Intacs. Dr. Hersh is conducting a study in which one group receives a combination procedure consisting of Intacs, then CXL, on the same day. The other group receives Intacs first, followed by CXL three months later. “We want to answer two questions,” Dr. Hersh said. “Are they compatible? And is there a difference in outcomes if the procedure is timed differently?”
Early findings on 43 patients suggest the procedures are compatible, with encouraging results, he said. The combination achieves a similar amount of flattening whether the procedures are concurrent (5.84 D) or sequential (5.34 D). Although the study is ongoing, early results do not show a difference in outcomes between the two groups.
Dr. Rabinowitz has also been studying how best to employ the techniques of CXL and Intacs. He recommends CXL alone in a young person who is progressing rapidly. If a patient isn’t progressing much but wants to improve vision, he inserts Intacs. If he wants to stop progression and improve vision, he would use both—but in separate procedures. “I can do [either] CXL or Intacs first,” he said, but either way, he prefers waiting three months between procedures. “Two procedures at once confound the outcomes.” However, he is continuing to research the additive effects, timing, and sequence of this combined modality.
CXL plus custom PRK. Dr. Lin and Simon P. Holland, MD, have performed more than 1,100 cases of combined PRK and CXL, mostly with the WaveLight Allegretto Wave excimer laser (Alcon). TG-PRK normalizes the corneal shape anatomically, Dr. Lin said. But smoothing any cornea induces a refractive change, which needs to be corrected. CXL also flattens the cornea, causing other refractive changes. The result of the combination treatment is a perfect-looking cornea, he said. “They’re really smooth, but the refractive result is way off.”
To counteract the problem of hard-to-predict induced refractive changes, Drs. Lin and Holland developed a method called custom topographic neutralization technique (TNT). They have reported on 217 eyes that underwent custom TNT TG-PRK in a combined procedure, with the PRK first, followed by CXL.3 Many of their patients were awaiting corneal transplants. More than half (59 percent) of the 72 eyes that completed 12-month follow-up had uncorrected distance visual acuity 20/40 or better, while 92 percent achieved best-corrected distance visual acuity of 20/40 or better.
“We can get people close to functional vision without glasses,” Dr. Lin said, adding that most of the patients who underwent combined custom TNT and CXL have been able to avoid transplantation.
For now, their method isn’t readily transferable to other practices. “All the finesse is to figure out how to put the refractive component into your treatment. It’s a very multifactorial approach regarding refractive error,” Dr. Lin said, adding that it took five years to develop the algorithm and “another three to four to smooth it out.”
Athens protocol. A similar procedure combining TG-PRK and CXL is known as the Athens protocol. At the 2012 Joint Meeting, Anastasios John Kanellopoulos, MD, presented the results of six to 48 months of follow-up in 212 eyes with keratoconus. None of the eyes demonstrated progression during the study, and there was an improvement in mean keratometry readings from 51.5 D to 47.5 D. Fifty percent of cases gained two lines of corrected distance visual acuity, while 35 percent gained three lines.4
CXL plus microwave. Dr. Hersh is recruiting 130 patients for a randomized controlled study comparing the Vedera KXS Microwave System (Avedro) in combination with CXL to CXL alone. The device delivers a single low-energy microwave pulse lasting less than one second. A single pulse raises the temperature of the selected region of corneal stroma, shrinking the collagen and forming a toroidal lesion in the upper 150 µm of the stroma. The lesion is intended to flatten the central cornea without compromising its biomechanical integrity. Early results show a marked flattening of the cornea, but the patients need to be followed for a longer time to determine stability of the results, Dr. Hersh said.
CXL plus phakic intraocular lenses. Two types of PIOLs are approved for refractive use (but not for keratoconus) in the United States: the Visian Implantable Collamer Lens (ICL; Staar) and the Verisyse (Abbott Medical Optics). These devices may be useful in cases of high myopia when laser treatment isn’t indicated because the cornea is too thin. However, because these devices require intraocular surgery, they are more invasive than the options described above.
Refer Your Patients to a Trial
In April 2009, EyeNet reported that FDA approval of CXL was imminent pending final review of a multicenter clinical trial. CXL still awaits approval, but some progress is being made. In 2011, Avedro was granted FDA orphan designations for CXL in the treatment of two conditions: keratoconus and corneal ectasia following refractive surgery, paving the way for doctors to perform CXL in trial settings. Subsequently, in March 2012, the company announced that it had submitted a new drug application to the FDA for its VibeX/KXL cross-linking system for those indications.
Today, ophthalmologists who can perform CXL are located in all the major U.S. cities, Dr. Trattler said. “There is no reason a patient should have to wait for FDA approval.”
Dr. Rabinowitz agreed. “If I had a kid rapidly progressing, I would want to have this treatment for them. It’s available in Canada and multiple sites in the United States, including our own site, where we have treated over 300 patients, including 40 in the pediatric age group.”
At the time of publication, 15 actively recruiting U.S. studies of CXL for keratoconus were listed on www.clinicaltrials.gov. The trials, which are evaluating several of the treatment approaches discussed in this article, range from single-site to multicenter studies with up to 49 sites.
Check the following websites for further information on clinical trials:
www.clinicaltrials.gov (enter “keratoconus” in search field)
www.nkcf.org/cxl-sites-2013/
www.keratoconuscenter.com/site/clinical-trials.htm
www.keratoconus.com/7.html
|
Picking and Choosing
Which combination is right for your patient? Dr. Hersh has seen good results with both CXL plus PRK and CXL plus Intacs. “These are decidedly different technologies to improve corneal stability and contour. We’ll learn how to best combine them for the most optimal outcome.” But questions remain, he said. “How do they work together? What is the timing? Those are the things that, as we learn [more] over the years to come, will improve our treatment of keratoconus markedly.”
William S. Trattler, MD, a surgeon at the Center for Excellence in Eye Care, in Miami, performs CXL as a first-line treatment. If patients need more, he prefers custom PRK over Intacs. “With the laser, you may see better with spectacles and not need contact lenses,” he said. He added that since Dr. Seiler introduced CXL, lots of variations have been introduced that shorten procedure time and/or improve efficacy. “We still don’t know the best order or combination. It’s not that there are any bad choices. We know they all work well. But we may fine-tune and improve.”
Dr. Rabinowitz predicted that these treatments will cut down on corneal transplants and that treatment will begin earlier. Dr. Lin agreed. “If you can catch keratoconus early and treat it, that’s the way to go.”
___________________________
1 Wollensak G et al. J Cataract Refract Surg. 2003;29(9):1780-1785.
2 Hersh PS et al. J Cataract Refract Surg. 2011;37(1):149-160.
3 Lin DTC et al. J Refract Surg. 2012;28(11 suppl):S841-S848.
4 Kanellopoulos AJ. Long-term follow-up of the Athens protocol: combined topography-guided partial PRK and corneal crosslinking in 212 keratoconus eyes. Presented at: AAO-APAO Joint Meeting; Nov. 12, 2012; Chicago.
___________________________
Dr. Hersh is a consultant for Avedro in his capacity as medical monitor for their clinical trials. Dr. Lin reports no related financial interests. Dr. Rabinowitz has no financial interest in the technologies described above. He receives support from the National Eye Institute for his research on keratoconus (NEI 09052). Dr. Trattler is a consultant to CXLO and CXL-USA.