Download PDF
Researchers at the Stein Eye Institute in Los Angeles have identified 2 risk factors significantly associated with low intraocular pressure (IOP) after trabeculectomy—the use of laser suture lysis and the individual surgeon.1 However, patients with and without low IOP had similar rates of reoperation, vision loss, and overall surgical failure.
“Developing low postoperative IOP does not necessarily equate with developing clinical signs of hypotony that threaten vision,” said Victoria L. Tseng, MD, PhD, at Stein Eye Institute.
Study details. Dr. Tseng and her colleagues compared 64 cases of low IOP to 130 controls without low IOP. Low IOP was defined as IOP ≤ 5 mm Hg on 3 or more consecutive visits after surgery. Cases were drawn from 3,659 trabeculectomies performed by 5 surgeons between 1990 and 2013.
Assessing risk. Laser suture lysis was negatively correlated with postsurgical low IOP. Only 28.1% of low IOP cases had undergone the procedure, versus 50.8% of controls. This is not to say that the procedure was protective against hypotony, Dr. Tseng said. Rather, laser suture lysis patients had a higher mean baseline IOP and thus had farther to fall following surgery, she explained.
The second risk factor—the clinician who performed the surgery—was positively correlated with low IOP after trabeculectomy. This association is likely due to patient selection, with 1 surgeon operating on a higher proportion of patients with lower baseline IOP than the others, Dr. Tseng said. Surgical technique was probably not a factor, since the surgeons followed a similar protocol.
Bottom line. The factors associated with low IOP are likely proxies for patients requiring a lower target IOP, said Dr. Tseng. The low postoperative IOP “may have been somewhat intentional.” Her advice: “The assessment of a patient’s progress after surgery and the need for further procedures should be based on a full clinical assessment and not IOP alone.”
—Miriam Karmel
___________________________
1 Tseng VL et al. Ophthalmology. Published online June 11, 2017.
___________________________
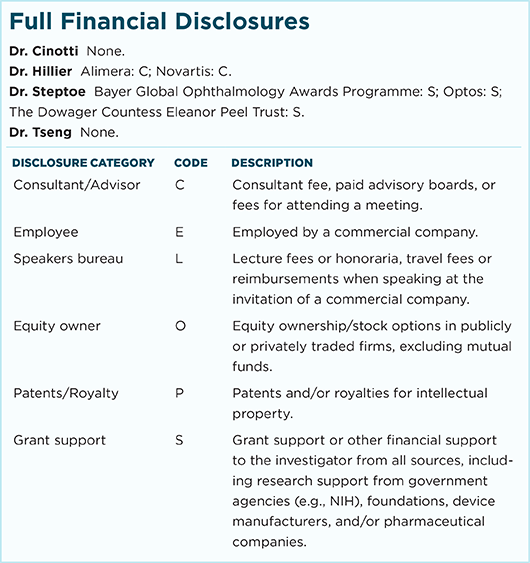
Relevant financial disclosures—Dr. Tseng: None.
For full disclosures and disclosure key, see below.
More from this month’s News in Review