By Annie Stuart, Contributing Writer, interviewing Eric Eggenberger, DO, Steven L. Galetta, MD, Daniel Gold, DO, and Janet C. Rucker, MD
Download PDF
Nystagmus—a spontaneous, repetitive, to-and-fro movement of the eyes—can be difficult for clinicians to categorize accurately. “It may be challenging to see the patient’s eyes move quickly in real time and understand what is going on,” said Eric Eggenberger, DO, at Michigan State University in East Lansing.
The next clinical challenge? Deciding which “machinery” is malfunctioning—and what treatment to order.
 |
|
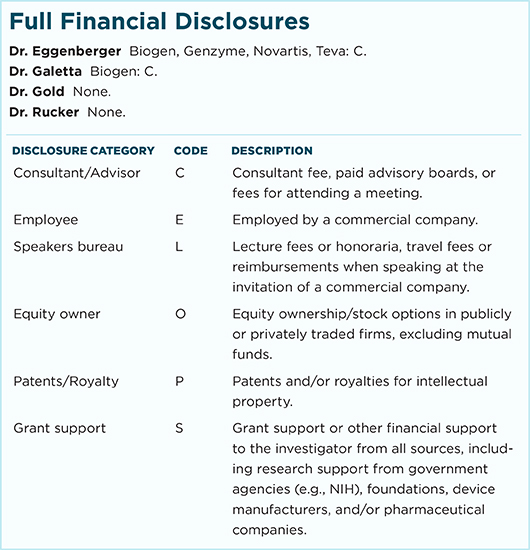
EVIDENCE ON MRI. Hyperintensity (arrow) within the right medulla of a patient with MS who presented with upbeat (central vestibular) nystagmus.
|
Is It Really Nystagmus?
The 2 main types of acquired adult nystagmus are jerk, named for its fast corrective phase, and pendular, which has slow back-and-forth phases, said Janet C. Rucker, MD, at NYU Langone Medical Center in New York City.
First, rule out the mimics. Before deciding on the type of nystagmus, there’s an even more important question, said Daniel Gold, DO, of Johns Hopkins Medicine in Baltimore: Could it be another kind of oscillation? Possible mimics include ocular flutter and opsoclonus, which often are due to etiologies that are not benign, such as cancer or an underlying infection or inflammatory condition (see “Online Tutorials”).
Then, pin down the origin. The main job for the clinician is to determine if the nystagmus is caused by peripheral vestibular disease or by involvement of the brainstem and cerebellar connections, said Steven L. Galetta, also at NYU Langone Medical Center.
Looking for associated signs can be helpful: Associated hearing loss favors a peripheral location, while saccadic pursuit abnormalities or a skew deviation strongly suggest a central etiology. Acquired pendular nystagmus (APN) and pathological gaze-evoked nystagmus usually also have a brainstem or cerebellar localization (see “Define Your Terms”).
 |
|
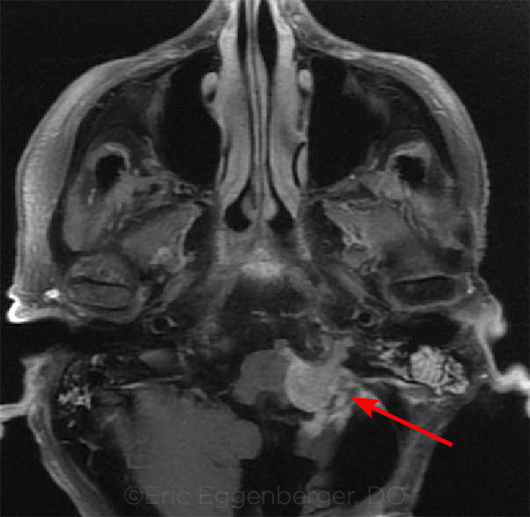
ROOT CAUSE. Recurrent meningioma (arrow) in a patient with vestibular and gaze-evoked nystagmus.
|
The Diagnosis
“Localization tells you where the problem is but, by itself, won’t tell you what the problem is,” said Dr. Eggenberger. “For that, you need to also look at the patient’s demographics and history and other details of the exam and testing.”
History. Ask about the time of onset and whether the nystagmus is continuous or episodic, as well as about any associated features, said Dr. Eggenberger. The cardinal symptom tied to nystagmus is oscillopsia, he said, but be sure to check for any central symptoms.
To uncover potentially serious dietary issues, ask about a history of bariatric surgery or heavy alcohol use—both are associated with several nutritional deficiencies (notably, deficiencies of vitamins B1 and B12) that can cause nystagmus. A recent head or neck injury could also dissect a vertebral artery, causing stroke, said Dr. Gold, and severe headache might point to hemorrhage in the posterior fossa.
Eye and physical exam. A full neuro-ophthalmic exam checks not only acuity but also color perception and visual fields, with a focus on motility, said Dr. Eggenberger.
Dr. Gold recommends taking the following steps:
- First, check for presence of spontaneous nystagmus—ophthalmoscopy can make subtle nystagmus easier to appreciate.
- Then, evaluate for nystagmus in each direction of gaze, especially to see if it’s unidirectional (which usually indicates a peripheral vestibular disturbance) or bidirectional (which is always central).
- Use alternate cover testing, especially to evaluate for a skew deviation, which is commonly present with posterior fossa pathology.
- Check smooth pursuit and saccades. Saccadic dysmetria also suggests a central etiology. Smooth pursuit can be difficult to assess when significant nystagmus is present, but if vertical pursuit is abnormal when the patient has spontaneous horizontal nystagmus, this is likely a central etiology.
- When vertigo accompanies nystagmus and lasts hours to days, the vestibulo-ocular reflex (VOR) may be assessed with the head impulse test (commonly performed by neurologists). VOR is usually impaired with peripheral etiologies and spared with central etiologies.
“One of the most important things to figure out is whether or not jerk nystagmus is pathologic or even physiologic,” said Dr. Galetta. “It’s not uncommon for a normal patient to have a few beats of jerk nystagmus in lateral gaze. Physiologic nystagmus often fatigues with prolonged eccentric gaze and is of low amplitude. If there’s more than 5 degrees of nystagmus amplitude, however, it’s likely pathologic. If the nystagmus appears different in right and left gaze, it’s clearly abnormal.”
Is neuroimaging necessary? The following questions may point you toward neuroimaging.
Is it a peripheral presentation? A unidirectional jerk nystagmus with a positive head impulse test, no skew deviation, and recent acute onset of vertigo suggests a peripheral vestibular disturbance, said Dr. Gold.
When a peripheral etiology is suspected, added Dr. Eggenberger, look for a mixed pattern of nystagmus such as torsional horizontal, in which the slow phase rotates toward the ear with hearing loss. “That’s how you will decide which side is the problem, may suspect vestibular neuritis, or will elect to do a scan to make sure it’s not a cerebellar stroke that’s mimicking peripheral vestibular nystagmus.”
Is it a central presentation? “If the nystagmus changes direction, there’s a skew, or the head impulse test is negative, you might be dealing with a central disorder such as a stroke, and the patient will require imaging,” said Dr. Galetta. And if any central symptoms or signs are elicited, then imaging should always be done, added Dr. Gold.
“Let’s say a 30-year-old patient has an ataxia presentation with oscillopsia,” said Dr. Eggenberger, “and on exam you find downbeat nystagmus in lateral gaze.” If you suspect multiple sclerosis (MS), he said, you might proceed with magnetic resonance imaging (MRI). Other specialists might then follow up with a spinal tap or other testing, depending upon what the MRI revealed.
By contrast, you might consider a degenerative process in an 80-year-old male with a slowly progressive history, said Dr. Eggenberger. “In that setting, you might look for vitamin deficiencies or other potential mimics. You would likely image and might consider genetic testing,” possibly for hereditary ataxias.
Is it a gaze-evoked presentation? If the presentation is symmetric—the patient looks to the left and you see a few beats; then looks to the right and you see a few beats—it is likely physiologic gaze-evoked nystagmus, which is common and doesn’t require any further evaluation, said Dr. Eggenberger. “On the other hand, if it is asymmetric, there is a problem in the gaze-holding mechanism somewhere in the left part of the brainstem.”
With any central pattern, added Dr. Gold, neuroimaging is always needed to rule out a structural abnormality.
Referral. Depending upon what your evaluation uncovers, said Dr. Eggenberger, you may refer to neuro-ophthalmology, otolaryngology, or neurology. In any case, the experts recommend that you refer the patient for any unexplained findings.
If you see signs of an acute stroke, make an urgent ER referral. Although most of these patients tend to go directly to the ER, Dr. Gold said, some do show up first in the ophthalmologist’s office, especially if their vertigo is not severe. That’s because the patient often perceives oscillopsia as an eye problem, rather than an ear or a brain issue. It’s also important to remember, Dr. Galetta added, that nystagmus is sometimes the only sign of a stroke.
Define Your Terms
Peripheral Vestibular: Jerk Nystagmus
This type of nystagmus is generated by vestibular asymmetry, and it can be due to an inhibitory disorder like vestibular neuritis or an excitatory disorder like benign paroxysmal positional vertigo (BPPV), said Dr. Gold.
Pattern. This type of nystagmus always beats in one direction, said Dr. Galetta. It also tends to have a mixed pattern, said Dr. Eggenberger, such as torsional horizontal or torsional vertical.
Symptoms. Many patients present with vertigo and dizziness as well as nystagmus, Dr. Eggenberger said.
Common causes. When BPPV is to blame, patients complain of vertigo and/or oscillopsia triggered by head movements, said Dr. Gold. However, it’s difficult to confirm the diagnosis without eliciting the typical pattern(s) of nystagmus that would be expected with positional maneuvers, such the as Dix-Hallpike test.
Vestibular neuritis causes unidirectional nystagmus in accordance with Alexander’s law—the nystagmus will increase in the direction of the fast phase, said Dr. Gold. “If it’s right-beating nystagmus, for example, it will increase in intensity when the patient looks to the right.” (However, he added, the nystagmus associated with a unilateral central vestibular lesion may also obey Alexander’s law.)
Central Vestibular: Jerk and Pendular Nystagmus
Pattern. Central vestibular nystagmus often involves vertical waveforms (upbeat or downbeat) or pendular waveforms, with back-to-back slow phases, said Dr. Eggenberger. APN may have horizontal, vertical, and/or torsional components, said Dr. Rucker.
Symptoms. If the brainstem is involved, associated central symptoms may include double vision, slurred speech, hemiparesis or hemisensory loss, ataxia, hearing loss, hiccups or hoarseness, or difficulty swallowing, said Dr. Gold. If the patient has had a stroke, the spontaneous nystagmus is often accompanied by acute-onset, prolonged vertigo lasting hours or days.
APN is often highly visually disabling, Dr. Gold said. In a patient with MS, APN may be asymmetric if there is a history of optic neuritis with poor visual recovery in one eye, Dr. Rucker added.
Common causes. Anything affecting the central wiring can cause central vestibular nystagmus, said Dr. Eggenberger, including stroke, MS, demyelination, trauma, neoplasms, tumors, or degenerative processes. In addition, he said, Wernicke’s encephalopathy from vitamin B1 deficiency is a treatable cause of upbeat nystagmus.
Gaze-Evoked Nystagmus
“Gaze-evoked nystagmus often reflects an inability of the brain’s neural integrator to keep the eye locked in an eccentric position and prevent it from drifting back toward center,” said Dr. Eggenberger.
Pattern. Gaze-evoked nystagmus is very common and is elicited only in eccentric gaze, said Dr. Rucker. It includes both physiologic and pathologic forms. The pathologic type has a sustained, larger amplitude.
When the neural integrator isn’t working and a patient looks to the right, for example, Dr. Gold said, the orbital elastic tissues move the eyes back to center (slow phase of nystagmus), and a rightward fast phase is generated to keep the eyes looking to the right.
Common causes. “Gaze-evoked nystagmus is commonly related to medications, such as antiseizure medications, especially at higher blood levels,” said Dr. Gold. “But anything that affects normal functioning of the posterior fossa may cause it, such as infection, inflammation, tumor, stroke, or MS.”
|
Treatment
The goal of therapy for nystagmus, said Dr. Eggenberger, is to treat the underlying cause, which will often take care of ocular manifestations, especially with many of the peripheral vestibular disorders. (In the vast majority of cases, Dr. Gold added, horizontal jerk vestibular nystagmus will resolve over days or weeks as the brain’s vestibular system recalibrates.) If it’s not possible to successfully treat the underlying cause, the goal is to manage symptoms.
Medical. Drug treatments to consider include the following.
- Baclofen can be very helpful for periodic alternating nystagmus (PAN), a distinct form of central vestibular nystagmus that switches from one side to the other approximately every 90 to 120 seconds,1 Gold said.
- Botulinum toxin (e.g., Botox) is occasionally used to quiet nystagmus, but it can cause double vision and ptosis, Dr. Galetta said.
- Chlorzoxazone may be helpful for downbeat nystagmus.
- Dalfampridine is expensive and is often not approved by insurance for downbeat (and occasionally upbeat) nystagmus. As a result, it must be procured via compounding pharmacies as 4-aminopyridine.1
- Gabapentin and memantine have been tested and studied for APN. “Used off label, gabapentin can be highly effective in decreasing oscillopsia and nystagmus amplitude,” said Dr. Rucker.
Optical or mechanical. In some patients, the use of prisms can stimulate convergence mechanisms, which can quiet the nystagmus pattern. In others, contact around the eye—either through touch or a contact lens—can achieve the same result.
Surgical. Mainly conducted in centers with special expertise, eye muscle surgery might be considered when drugs are ineffective and the nystagmus is intractable, said Dr. Galetta.
___________________________
1 Kalla R et al. J Neurol. 2016;263(suppl 1):24-29.
___________________________
Dr. Eggenberger is professor and vice chairman of neurology at Michigan State University in East Lansing, Mich. Relevant financial disclosures: None.
Dr. Galetta is professor and chair of neurology and professor of ophthalmology at NYU Langone Medical Center in New York, N.Y. Relevant financial disclosures: None.
Dr. Gold is assistant professor of neurology, ophthalmology, neurosurgery, and otolaryngology at Johns Hopkins Medicine in Baltimore, Md. Relevant financial disclosures: None.
Dr. Rucker is professor of neurology and director of the neuro-ophthalmology division at NYU Langone Medical Center in New York, N.Y. Relevant financial disclosures: None.
For full disclosures and the disclosure key, see below.