Download PDF
Decreased lubrication of the ocular surface due to inadequate eyelid closure or decreased blink frequency can lead to exposure keratopathy. This review will discuss the diagnosis and treatment of this form of dry eye syndrome.
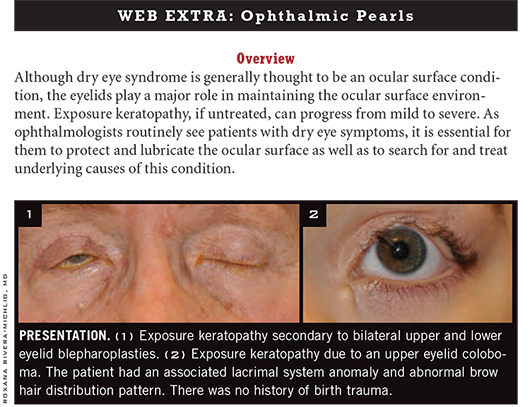
Overview
Symptoms and signs. Common symptoms of exposure keratopathy include pain, foreign body sensation, epiphora, photophobia, and blurry vision. Patients with decreased corneal sensation may experience minimal nociceptive symptoms. Common signs include incomplete blink, lagophthalmos, decreased tear meniscus, decreased tear film breakup time, corneal filament formation, punctate epithelial erosions, and epithelial defects. In severe cases, corneal edema, thinning, and ulceration may develop.
 |
|
SYSTEMIC. Paralytic lagophthalmos caused by right cranial nerve VII palsy.
|
Diagnosis
Exposure keratopathy is a clinical diagnosis based on history and physical examination findings. Patients frequently present with a presumed diagnosis of “dry eye,” but ophthalmic examination reveals that corneal exposure is the underlying etiology.
Eyelids. Careful examination of the eyelids is necessary to evaluate for possible malposition. A history of eyelid trauma or surgery, including blepharoplasty, should be elicited. The eyelids should be examined for ectropion, entropion, or retraction. The eyelid contour should be evaluated for evidence of notching that may occur in patients with congenital colobomas, severe blepharitis, or a history of eyelid laceration, either from trauma or surgery.
Lagophthalmos, decreased blink frequency, and weakened orbicularis strength are also important, and are typical features of Bell palsy. Eyelids should be everted to evaluate the palpebral conjunctiva. If the eyelids are everted easily, especially in patients with a history of sleep apnea or snoring, floppy eyelid syndrome may be the underlying etiology.
Proptosis. This can lead to exposure keratopathy even in the presence of normal eyelids and can exacerbate exposure keratopathy in the setting of eyelid anomalies. Proptosis can be measured either by Hertel exophthalmometry, which provides a quantitative measurement that can be followed over time, or by viewing from the top, past the patient’s forehead.
Proptosis may be exacerbated by eyelid retraction in thyroid eye disease. Blood tests, such as those for thyroid-stimulating hormone and thyroid-stimulating immunoglobulin, should be ordered, especially when the proptosis is associated with eyelid retraction and lid lag. Imaging studies may be indicated to evaluate for enlargement of the extraocular muscles related to thyroid orbitopathy or orbital myositis as well as to evaluate for orbital masses.
Systemic issues. Herpetic keratopathy and damage to the ophthalmic branch (V1) of cranial nerve V can decrease corneal sensation, which can be evaluated in the clinic using an esthesiometer or a wisp of cotton prior to instillation of topical anesthesia. Overuse of oral or topical pain medication may also contribute to decreased corneal sensation and decreased blink frequency. Cranial nerve VII palsy can lead to incomplete blink and paralytic lagophthalmos (Fig. 1). Movement disorders, such as Parkinson disease and progressive supranuclear palsy, may decrease the blink rate and cause exposure keratopathy, highlighting the importance of observing the patient’s blink rate.1
(Click to expand)
Treatment
Treatment varies according to disease severity and underlying etiology. For instance, if an eyelid malposition, notch, or coloboma is the cause of exposure, medical therapies may be considered as temporizing measures until the eyelid can be repaired surgically. In severe cases with corneal ulceration, cultures and sensitivities may be indicated to rule out an infectious component or to guide antibiotic therapy.
Lubrication and plugs. Mild cases of exposure keratopathy are characterized by punctate epithelial erosions, often confluent, within the palpebral fissure. Our preferred treatment in such cases is lubrication using ointments, starting with ointments containing antibiotics such as erythromycin and eventually transitioning to bland artificial tear gels. We advocate early placement of long-acting collagen or silicone punctal plugs to assist in retention of natural lubrication with minimal risks and complications.
Steroids. Use of weak topical steroids (such as loteprednol 0.2 percent) can be employed to provide short-term symptom relief; however, caution is needed due to the risk of exacerbating corneal ulcerations that may occur with exposure keratopathy. Subsequently, it may be difficult to wean some patients off steroids.
Amniotic membrane. Amniotic membrane can be applied via a single device composed of amniotic membrane encased between two synthetic rings (ProKera; Bio-Tissue) or attached using fibrin glue or sutures. However, as the amniotic membrane is temporary and use of multiple membranes in succession is costly, we try not to use this for long-term therapy. Amniotic membrane is especially useful in patients who either are reluctant to undergo tarsorrhaphy or are unable to tolerate tarsorrhaphy with local anesthesia only and thus need to be scheduled for monitored anesthesia care in an operating room.
Bandage and scleral contact lenses. In select cases, cautious use of bandage contact lenses, with concurrent broad-spectrum antibiotic coverage to reduce the risk of corneal ulcers, may be necessary. We do not advocate this treatment as a long-term option because of the change in the ocular surface flora that results from long-term antibiotic administration and the risk of infection, including fungal.
Scleral contact lenses, such as the prosthetic replacement of the ocular surface ecosystem lens (PROSE; BostonSight), can be sight saving for patients with severe ocular surface disease. However, even though the FDA approved PROSE lenses in 1994 for the treatment of ocular surface disease and ectasia, not all insurance companies cover the devices.
Moisture chamber or eyelid taping. This may be useful at night in moderate to severe cases of exposure keratopathy, or in patients who refuse tarsorrhaphy. An effective and low-cost moisture chamber can be made using plastic wrap, which is adhered to the skin using ointment, to provide an airtight seal between the skin and plastic wrap. One technique begins with the application of ointment to the inferior fornix; ointment may then be applied in a continuous circle along the skin of the superior, lateral, and inferior orbital rim as well as the lateral aspect of the nose. The plastic wrap, cut to shape, can then be placed over the ointment.
Eyelid taping may be performed by first applying ointment to the inferior fornix of the eye. An eye pad is then placed on the eye, and paper tape is used to hold this in position with upward traction on the cheek. If this does not provide adequate closure, a piece of tape can be applied horizontally from the upper eyelid margin down to inferior orbital rim, taking care to avoid getting ointment on the tape.
Tarsorrhaphy. More definitive therapy consists of tarsorrhaphy. In general, we prefer reversible marginal tarsorrhaphy as a first step. This can be lateral tarsorrhaphy, lateral and medial tarsorrhaphy, or complete tarsorrhaphy. The last is appropriate for severe cases in which complete occlusion of vision is functionally acceptable.
Bolstered tarsorrhaphies are particularly useful in patients with corneal ulcers or other surface disease that requires frequent examination.
Reversible tarsorrhaphy technique. We inject the eyelid margin with 1 percent lidocaine with epinephrine. We then use fine-toothed forceps to hold the upper eyelid margin, full-thickness, and we use a #11 blade or Westcott scissors to remove a thin strip of lid margin epithelium behind the eyelashes, the length of which corresponds to the desired tarsorrhaphy length. This is repeated for the lower eyelid. Sutures (5-0 or 6-0) are then placed in a horizontal mattress fashion. The eyelid is dressed with a steroid-antibiotic ointment for seven to 10 days.
Bolstered tarsorrhaphy technique. The eyelid margin is injected with 1 percent lidocaine with epinephrine. The lid margin epithelium is denuded as described above. Nylon suture is used to place a horizontal mattress suture. First, the needle is passed through the bolster material (pieces of tubing from a 25-gauge butterfly needle work well). Then, the lateral lower eyelid pass is placed, entering below the lower eyelash line but engaging the tarsal plate and exiting at the gray line, followed by the upper eyelid pass, which enters at the gray line, engaging the tarsal plate, and exiting above the upper eyelash line. After traveling 4 to 5 mm medially, the suture is passed from upper eyelid to lower eyelid. Finally, the suture is again passed through the bolster material and tied.
If the tarsorrhaphy needs to be adjustable so that it can be opened to allow examination of the ocular surface, then space is left between the bolster and the lower eyelid margin prior to tying off the suture. The marginal tarsal epithelium should not be removed to allow opening of the palpebral fissure for ocular examination.
___________________________
1 Karson CN et al. Neurology. 1984;34:677-678.
___________________________
Dr. Rajaii is a fellow in oculoplastic and reconstructive surgery at the University of Michigan, Ann Arbor, and Dr. Prescott is assistant professor of ophthalmology at Wilmer Eye Institute. The authors report no financial interests.