By Yu Qiang Soh, MD, Daniel S.W. Ting, MD, PhD, and Edmund Y.M. Wong, FRCS(Ed)
Edited By: Sharon Fekrat, MD, and Ingrid U. Scott, MD, PhD
Download PDF
The crystalline lens is normally held in a stable intraocular position by zonular fibers that connect to the ciliary body and attach circumferentially to the equatorial region of the lens capsule. Similarly, placement of an intraocular lens (IOL) into the capsule after cataract removal provides anatomical support to the IOL. However, damage to the zonular- capsular complex from trauma or disease can lead to structural weakness and loss of lens stability. Severity may range from mild phacodonesis or pseudophacodonesis to partial subluxation and even complete lens dislocation, into either the anterior or posterior segment.
An anteriorly dislocated crystalline lens or IOL is often considered to be an ocular emergency because of the risk of lens-induced angle-closure glaucoma and corneal damage.
In contrast, posterior dislocation usually involves comanagement with a vitreoretinal surgeon for consideration of vitrectomy and removal of the dislocated lens or IOL through a pars plana approach. If the posteriorly dislocated crystalline lens is intact, it may be observed in some cases. Some eyes with posteriorly dislocated lens or IOL may be left aphakic.
In this article, we focus on the diagnosis and management of posteriorly dislocated crystalline lenses and IOLs.
 |
|
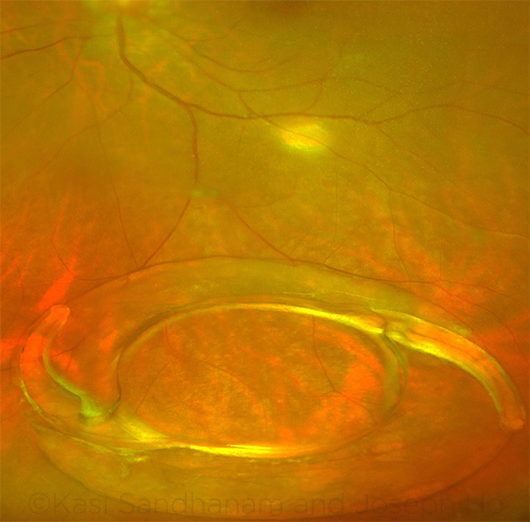
DISPLACED IOL. Fundus photograph shows a posteriorly dislocated intraocular lens with the capsular bag in the vitreous.
|
Risk Factors
Risk factors may be divided broadly into congenital or acquired categories. In systemic disorders, dislocation is usually bilateral.
Congenital. Systemic. Marfan syndrome, which is a systemic connective tissue disorder, is the most common congenital cause of crystalline lens dislocation. A mutation in the FBN1 gene renders the zonules weak and lax, leading to lens subluxation or dislocation, classically in the superotemporal direction.
Homocystinuria, the second most common congenital cause, is associated with brittle zonules, which can result in inferonasal lens subluxation or dislocation.
Other important congenital etiologies include Weill-Marchesani syndrome, sulfite oxidase deficiency, hyperlysinemia, and congenital ectopia lentis et pupillae.
Ocular. Pseudoexfoliation syndrome, associated with a mutation in the LOXL1 gene, can cause repetitive chafing of the midperipheral iris against lens zonules, leading to phacodonesis and increased risks of iatrogenic zonulysis during phacoemulsification.
Acquired. Trauma. Ocular trauma is a common cause of acquired posterior lens dislocation. Whether it occurs in the form of closed- or open-globe injury, trauma may be associated with multiple other complex injuries such as retinal detachment, intraocular foreign bodies, and corneoscleral laceration, leading to difficulties in surgical repair and visual rehabilitation.
Even if frank phacodonesis is not apparent immediately after the trauma, such patients are at higher risk of sub-sequently developing progressive zonular dehiscence.
Myopia. Pathologic axial myopia is another important underlying etiology associated with acquired lens dislocation. It is especially relevant in the context of an East Asian population, owing to the prevalence of high myopia in this group.
Axial myopia inherently predisposes to zonular instability; in addition, myopia increases the risk of retinal detachment, and reparative vitreoretinal surgery may further weaken the zonular-capsular complex.
Inflammation. Persistent intraocular inflammation secondary to chronic uveitic conditions may similarly result in weakening of lens zonules.
Clinical Presentations
The patient may experience posture-dependent visual fluctuation, ocular pain, or headache from intermittent angle closure or intraocular inflammation preceding the occurrence of lenticular dislocation into the vitreous cavity.
After posterior lens dislocation, visual changes may range from a sudden decrease in visual acuity (VA) due to the loss of lenticular refractive power to a sudden improvement in VA secondary to a significant reduction in refractive error in a phakic myopic patient.
There may also be complaints of a “floater,” often in the superior visual field, corresponding to the dislocated crystalline lens or IOL settling in a dependent position within the vitreous cavity.
When assessing such symptoms, especially in the presence of the risk factors mentioned above, the ophthalmologist should maintain a high index of suspicion for lenticular dislocation and investigate further to ascertain the diagnosis.
Evaluation
In a patient with posterior lens dislocation, clinical evaluation and investigation should be directed at identifying the underlying etiology, evaluating the need for surgical intervention, and planning for surgical or optical rehabilitation.
Clinical exam. Detailed examination of the anterior segment should be performed, including the conjunctiva, sclera, cornea, angles, and iris. Dilated posterior segment examination with scleral depression, including assessment of the lens capsule, vitreous, and retina, is essential. Ultrasound B scan or, occasionally, ultrasound biomicroscopy may be useful for locating a lens posteriorly dislocated behind the iris around the vitreous base.
In or out of the capsular bag? In-the-bag dislocations suggest zonular weakness, whether primary or secondary, while out-of-the-bag dislocations are often associated with posterior capsular rupture during cataract surgery or other trauma.
Systemic evaluation. A thorough systemic examination is helpful in identifying characteristic features suggestive of connective tissue diseases, for example, the tall, lean habitus, hyperflexible joints, and cardiovascular anomalies associated with Marfan syndrome.
Conservative Management
In the absence of sight-threatening complications such as elevated IOP or corneal decompensation, conservative management may be an appropriate choice, especially for patients who have good vision in the fellow eye or are medically unfit for surgery. Such patients may be fitted with a contact lens for visual rehabilitation.
Follow-up needed. However, the ophthalmologist should perform regular clinical follow-up and remain vigilant for possible sequelae that might indicate a need for surgical intervention. These include increased intraocular pressure (IOP), bullous keratopathy, cystoid macular edema, retinal break, and retinal detachment. Patients who have high IOP should be referred to a glaucoma specialist.
Endothelial cell count and central cornea thickness measurement are useful for monitoring corneal health.
Surgery
In patients who have complications or bothersome symptoms, the typical approach involves pars plana vitrectomy (PPV) and removal of the dislocated lens, followed by secondary IOL implantation.
PPV. Using a standard 3-port vitrectomy setup, the surgeon performs an anterior and core vitrectomy to gain access to the posteriorly dislocated crystalline lens or IOL-capsule complex. Ideally, posterior vitreous detachment is induced (if not already present) and completed before the lens is manipulated to minimize unintended vitreoretinal traction.
Removal of the crystalline lens. For a dislocated crystalline lens, a fragmatome is inserted via a pars plana incision. The cataract or clear lens is emulsified in the midvitreous cavity using ultrasound.
Removal of the IOL. In the case of a posteriorly dislocated IOL, levitation of the IOL into the anterior chamber can be performed using end-gripping intraocular vitrectomy forceps.
Flexible IOLs can be cut with an IOL cutter in the anterior chamber under dispersive viscoelastic cover and removed via a corneal or sclerocorneal incision. Care must be taken to avoid trauma to the cornea, iris, and angles.
Rigid IOLs are usually removed through a larger scleral tunnel or sclerocorneal incision.
Secondary IOL implantation. In the absence of capsular support, the secondary IOL can be inserted into either the anterior or posterior chamber. The choice of techniques is highly dependent on patient, ocular, and surgeon factors. Corneal, scleral, and iris conditions (e.g., atrophy or traumatic aniridia) must be considered carefully to determine the appropriate method.
Anterior chamber placement. Implantation of an anterior chamber IOL (ACIOL), with fixation in the angle, is relatively quick, very stable, and less technically demanding than the other techniques. However, even with modern open-loop ACIOL models, angle-supported IOLs are associated with potential long-term risks such as corneal endothelial decompensation, glaucoma, and persistent intraocular inflammation.1
Posterior chamber placement. Many of the complications associated with ACIOLs can be avoided with use of retropupillary placement. The IOL may be placed in the posterior chamber with either iris or scleral fixation. However, these posterior chamber techniques are more surgically challenging and time-consuming, and are generally less stable, than ACIOL implantation.
Several variants of scleral fixation have been described,2-4 wherein the IOL haptics are either externalized and fixated intrasclerally or are secured intraocularly via nonabsorbable transscleral fixation sutures.
Conclusion
Lenticular instability leading to posterior subluxation or dislocation is a relatively common problem encountered in the practice of general ophthalmology. With timely detection and intervention, many of the potential complications can be avoided. Careful preoperative planning and intraoperative assessment of ocular and patient factors are essential to achieve excellent outcomes.
___________________________
1 Drolsum L. J Cataract Refract Surg. 2003;29(3):498-503.
2 Todorich B et al. Ocul Immunol Inflamm. Published online Oct. 11, 2016. doi:10.1080/09273948.2016.1231328.
3 El Gendy HA et al. J Ophthalmol. Published online Aug. 10, 2016. www.ncbi.nlm.nih.gov/pmc/articles/PMC4995346/.
4 McAllister AS, Hirst LW. J Cataract Refract Surg. 2011;37(7):1263-1269.
___________________________
Dr. Soh is an ophthalmology resident at Singapore National Eye Centre. Dr. Ting is an associate consultant in the Singapore National Eye Centre and assistant professor at the Duke-National University Singapore (NUS) Medical School. Dr. Wong is the head of the surgical retina department in the Singapore National Eye Centre and an adjunct associate professor at the Duke-NUS Medical School. Relevant financial disclosures: None.
More at the Meeting
Expand your techniques for managing IOLs that are malpositioned or lack capsular support with the following events.
An Innovative Approach to Iris Fixation of an IOL Without Capsular Support (Lab117). When: Sunday, Nov. 12, 10:00-11:00 a.m. Where: Room 350. Access: Ticket required. (Also presented as Lab126 on Nov. 12, 11:30 a.m.-12:30 p.m., in the same location.)
Management of Malpositioned IOLs (431). When: Monday, Nov. 13, 9:00-11:15 a.m. Where: Room 383. Access: Academy Plus course pass required.
|