By Dane H. Slentz, BS, and Houman D. Hemmati, MD, PhD
Edited by Ingrid U. Scott, MD, MPH, and Sharon Fekrat, MD
Download PDF
Stevens-Johnson syndrome (SJS) and its more severe variant, toxic epidermal necrolysis (TEN), are inflammatory disorders of the skin and mucous membranes that are characterized by acute, life-threatening blistering and necrosis. These conditions require extensive wound care, pain management, fluid and nutrition resuscitation, and respiratory support.
Initially, eye care is often superseded by the life-threatening dermatologic concerns. Nonetheless, the most common and devastating long-term complications often are ophthalmic in nature. As these complications can be minimized or even prevented with early intervention, an eye examination should be an essential component of the evaluation of any patient with suspected SJS/TEN. Despite this, patients may seek treatment from ophthalmologists many years after disease onset, well after the dermatologic changes have resolved and permanent visual impairment has occurred.1
The goal of this review is to offer strategies for managing the ophthalmic symptoms seen during the acute phase of SJS/TEN.
Overview
SJS and TEN are rare conditions; combined, they affect fewer than 8 cases per million persons per year.2 Age at disease onset varies widely; in a large series of 73 patients (138 eyes) with SJS, patients’ ages at onset ranged from 2 to 69 years.1
Signs and symptoms. Initially, patients develop a prodrome of unspecific symptoms that may include malaise, fever, headache, and cough. This is followed by an ill-defined rash that varies in extent and most commonly occurs on the face, neck, and upper trunk. The rash then blisters and sloughs off, with the skin’s appearance similar to that seen in large burns.
Typically, SJS affects less than 10 percent of the body’s surface, while TEN may denude more than 30 percent of the total body surface area. Involvement of 10 to 30 percent of the body surface area is called SJS/TEN overlap.3
Etiology. SJS and TEN are believed to be parts of a continuum of the same disease process. The proposed mechanism is not completely understood, but an autoimmune reaction seems to be involved.
Cases are typically linked to drug exposure. A number of medications have been implicated, including antibiotics (especially sulfonamides), anticonvulsants, nonsteroidal antiinflammatory drugs (NSAIDs), and antigout medications. Less commonly, cases may be related to infectious disease exposure, notably the herpes simplex virus and mycoplasma.
Genetic susceptibility may also be involved, as studies have found that the HLA-B12 gene is associated with a higher risk of the disease.4
Morbidity and mortality. The initial goal of managing suspected SJS/ TEN is to provide essential life support, as both conditions pose a significant risk of dehydration and infection during the acute phase, and admission to a burn unit may be necessary. Mortality rates range from 1 to 5 percent for SJS and up to 50 percent for TEN.3
 |
|
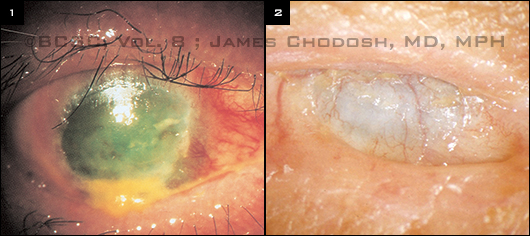
CLINICAL PROGRESSION. (1) The primary ocular finding is a mucopurulent conjunctivitis and episcleritis; bullae and extensive areas of necrosis may develop. (2) In this case of chronic, end-stage disease, severe scarring has resulted in scleralization and vascularization of the patient’s cornea. Note the absence of eyelashes and fusion of the eyelids (ankyloblepharon).
|
Ophthalmic Involvement
Acute. In the acute stages of SJS/TEN, more than 50 percent of patients experience ocular complications ranging from minimal to severe. Ocular surface inflammation develops rapidly at this stage and may be accompanied by pseudomembranous formation and/or corneal or conjunctival epithelial defects (Fig. 1).5
The acute ocular symptoms are due to goblet cell compromise in the conjunctival mucous membranes, which results in a destabilized tear film and associated ocular irritation from blink-related trauma. Hyperemia and/or chemosis occur due to involvement of the bulbar conjunctiva; involvement of the palpebral conjunctiva causes edema, erythema, and pseudomembrane formation.
Chronic. Inflammation and epithelial erosion often persist beyond the acute stage and the resolution of skin eruptions, leading to ocular complications and scarring in the chronic stage.1 Persistent epithelial defects, ulceration, and perforation may develop into corneal cicatricial changes such as neovascularization, opacification, keratinization, and symblepharon (Fig. 2). Depletion of limbal stem cells inhibits regeneration of the corneal epithelium.
Surgical correction may be employed to treat these chronic effects; however, the results are generally poor in terms of visual outcomes and quality of life. Permanent visual impairment and ocular discomfort may persist throughout life, and patients may require long-term medication and ophthalmic care.1
Characteristic ocular complications seen in the chronic stage may be assessed by the grading system developed by Sotozono et al.1 Of 13 possible long-term ocular complications assessed in this study, the most common were severe meibomian gland involvement and loss of the palisades of Vogt.
(click to expand)
Eye Care During Acute Phase
Early intervention during the acute phase of SJS/TEN decreases the risk of long-term ocular compromise.
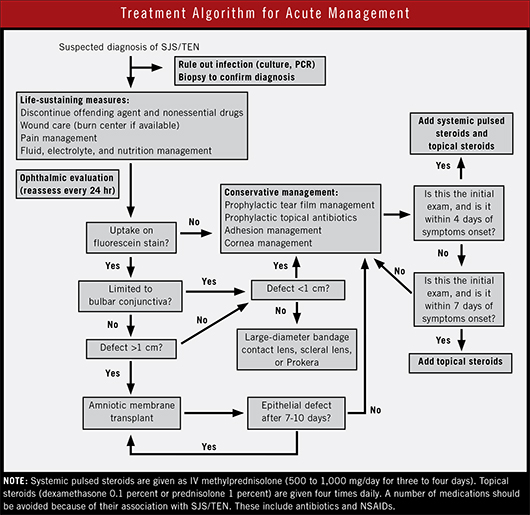
Initial examination. Normal saline should be applied to rinse away epithelial debris. Fluorescein staining should be used to assess for epithelial defects on the cornea, conjunctiva, and eyelid margins. At a minimum, all patients should receive adequate ocular lubrication with instructions on use of preservative-free artificial tear drops and ointments to reduce epithelial damage.
We recommend frequent (every one to two hours) use of preservative-free lubricating drops and application of a lubricating ointment, in addition to a topical fourth-generation fluoroquinolone, four times daily.
Daily follow-up care. Patients in the acute phase of SJS/TEN should have daily ophthalmic exams to monitor for disease status and signs of infection. Epithelial defects, corneal ulceration, and cicatricial changes, in addition to any other ocular complications, should be addressed promptly.
Fluorescein staining is a critical part of the daily exam, and special attention should be paid to the fornices, as these relatively hidden areas may be affected. Pseudomembranes and symblepharon should be lysed to deter cicatrization.
Small (<1 cm) epithelial defects that are limited to the bulbar conjunctiva, are nonprogressive, and do not have symblepharon should be treated conservatively. Large (>1 cm) epithelial defects that involve the lid margin, inferior palpebral conjunctiva, or ocular surface should receive an amniotic membrane transplant, or AMT (see below).
If surface dryness persists, punctal occlusion, partial tarsorrhapy, or autologous serum eyedrops may be considered. Corneal protection with a scleral lens may also be appropriate to prevent blink-related trauma.
Medications. Sulfonamide antibiotics and NSAIDs should be avoided, because of their association with SJS/TEN.
The role of steroids, especially systemic corticosteroids, during the acute phase is controversial. In one study, topical corticosteroids, when initiated during the first week of the acute phase, were found to improve vision.5 The topical steroids used in this study were dexamethasone 0.1 percent or prednisolone 1 percent, applied four times a day.
These findings were confirmed in a second study, in which researchers found that the combination of high-dose pulsed systemic steroids and topical steroids, when initiated within four days of disease onset, resulted in a significant reduction in ocular damage at the one-year mark. In this study, the researchers used intravenous methylprednisolone (500 to 1,000 mg per day for three to four days).6
However, corticosteroids may not be a viable option, as ophthalmic consultation may not be obtained within four days of disease onset, and the risk of infection increases with skin loss. Corticosteroid use should be considered in the context of the overall clinical picture, with attention to the fact that steroids may promote immunosuppression and worsen infection.
Amniotic membrane transplant. Recent evidence has supported the use of an AMT during the acute phase of SJS/TEN. Amniotic membranes exhibit anti-inflammatory and antiscarring properties that promote early wound healing.
A study of patients who had large (>1 cm) epithelial defects involving the lid margins, inferior palpebral conjunctiva, or ocular surface and who presented within 10 days of symptom onset had beneficial outcomes from AMT.2 Other studies have validated the use of AMT, with the greatest benefit occurring when AMT is performed within 72 hours of disease onset.7
Patients receiving AMT should undergo daily ophthalmic examinations, and the efficacy of the graft should be assessed seven to 10 days after surgery. An intact epithelium with minimal inflammation does not warrant another AMT; however, the persistence of epithelial defects may warrant placement of another graft. If eyelid margin involvement is absent or minimal, a subsequent AMT can be performed with the self-retaining amniotic membrane ring, Prokera (Bio-Tissue).
___________________________
1 Sotozono C et al. Ophthalmology. 2007;114(7):1294-1302.
2 Gregory DG. Ophthalmology. 2011;118(5):908-914.
3 Gerull R. Crit Care Med. 2011;39(6):1531-1532.
4 López-García J et al. Ophthalmology. 2011;118(2):265-271.
5 Sotozono C et al. Ophthalmology. 2009;116(4):685-690.
6 Araki Y et al. Am J Ophthalmol. 2009;147(6):1004-1011.
7 Ciralsky JB, Sippel KC. Clin Ophthalmol. 2013;7:1031-1034.
___________________________
Mr. Slentz is a medical student at the University of Vermont in Burlington and reports no related financial interests. At the time of writing, Dr. Hemmati was assistant professor of ophthalmology and surgery at the University of Vermont; he is now director of clinical development at Allergan. He reports no additional related financial interests.
Got Pearls
Write a Pearls Article!
Ophthalmic Pearls, EyeNet Magazine
655 Beach Street
San Francisco, CA 94109
eyenet@aao.org
Writers guidelines provided upon request.
ARE YOU A RESIDENT? A resident article will satisfy the RRC requirements for resident scholarly activity. |