By Diego Zamora-de la Cruz, MD, Marisol Garzón, MD, and Jesús Arrieta-Camacho, MD
Edited by Sharon Fekrat, MD, and Ingrid U. Scott, MD
Download PDF
Ocular trauma is relatively common. Up to one-fifth of adults will experience ocular trauma at some point in their lives. It occurs most frequently in men and young people.1 A study performed for the World Health Organization estimated that up to 55 million eye injuries occur annually worldwide, and up to 1.6 million people lose their sight due to eye trauma.2 In developed countries, it is a major cause of unilateral blindness.3
Various ocular structures can be damaged at the time of trauma; all patients who present with oculofacial trauma should be carefully examined to determine clinical and surgical management. Several guidelines for ocular trauma have been published to help determine the visual prognosis.4 Visual outcome generally depends on the initial visual acuity, pupillary reflex response, and severity of the trauma.
In this article, we will focus on the presentation and management of injury to the lens and, in particular, traumatic cataract.
Lens Trauma and Secondary Conditions
Trauma can affect the lens in several ways. For instance, it can be partially displaced from its natural position (subluxated) or completely dislocated (luxated).
Injury to the lens may lead to other ocular disorders through various mechanisms. For example, in phacomorphic glaucoma, the anteroposterior diameter of the lens swells to such a degree that it occludes the iridocorneal angle. Similarly, a subluxated or luxated lens can move forward, resulting in narrowing of the angle.
If the lens capsule is ruptured, lens proteins can impair aqueous outflow, either directly by clogging the trabecular meshwork (lens-particle glaucoma) or by causing an inflammatory response in the anterior chamber (phacoantigenic glaucoma).
Traumatic Cataract
Traumatic cataract is a clouding of the lens that may occur after either blunt or penetrating ocular trauma that disrupts the lens fibers.
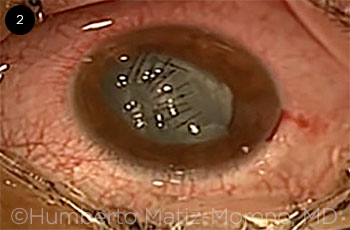
Most traumatic cataracts are intumescent, but their type and clinical course depend on trauma mechanism and the integrity of the capsular bag. The morphology of a classic traumatic cataract is referred to as a rosette or stellate type (Fig. 1).
 |
|
TRAUMATIC CATARACT. Characteristic stellate appearance of traumatic cataract.
|
Presurgical Considerations
Blunt or penetrating? The ophthalmologist should determine whether traumatic cataract is secondary to penetrating or blunt trauma.
Significantly low intraocular pressure (IOP) should always raise the suspicion of an open globe; however, in some cases, the wound self-seals, and IOP may be normal. If penetrating trauma is present, the use of topical medication or devices that touch the eye should be avoided. External pressure on the globe may cause extrusion of intraocular tissues, and environmental pathogens may lead to severe infections.
Once penetrating trauma has been ruled out, ultrasound A and B may be used to further assess ocular status. Ultrasound biomicroscopy or water bath immersion methods may also be used to visualize the posterior capsule.
Patient’s systemic health. Poorly controlled diabetes or systemic hypertension, for example, are associated with higher risk of perioperative and postoperative complications, including expulsive hemorrhage; diabetes is also associated with a higher risk of infection.
Choice of anesthetic. Anesthesia should be individualized for each clinical setting; some factors that influence the type of anesthesia are penetrating versus blunt trauma, patient age, health status, biometric characteristics of the eye, estimated duration of the procedure, and surgeon comfort.
It is usually preferable to employ general anesthesia in a patient with an open globe in order to reduce manipulation of the eye and pressure that may occur with ocular or periocular injection of anesthetic.
Aseptic and antiseptic procedures. The preoperative cleansing and sterilizing of the ocular area should be performed as carefully and gently as possible to avoid further damaging the eye or introducing bacteria into the eyeball.
Application of diluted povidone-iodine 5% in the conjunctival sac is the only method of antisepsis that has been demonstrated to significantly reduce the risk of endophthalmitis.5
Cornea
Laceration or loss of corneal tissue may be present as result of the trauma. A sealed anterior chamber is necessary to avoid fluid leakage during cataract surgery. Corneal wounds should be closed with 10-0 nylon suture, and this procedure may be done in the same surgical session as the cataract extraction.
Sutures should be placed in a perpendicular orientation starting from the edges if an irregular wound is present (Fig. 2).
The patient’s age will affect wound closure, as corneal elasticity changes with age. In pediatric patients, who have more elastic corneas, it is preferable to close the wound with higher tension rather than just apposing the tissue. This will prevent leakage of aqueous or solution during and after the cataract extraction procedure.
Effect on IOL calculation. A lacerated or traumatized cornea severely compromises intraocular lens (IOL) calculation, as it may be impossible to obtain an accurate keratometry measurement. In such cases, the surgeon may perform IOL calculation based on the fellow eye if it is uninjured or use a keratometry value of 44 D, representing an average value.
 |
|
CORNEAL REPAIR. Lacerations are sutured before cataract extraction.
|
Anterior Capsule and Zonules
Use of a capsular dye such as trypan blue helps the surgeon to visualize the anterior capsule in order to assess its condition and control it more easily.
Nonruptured anterior capsule. If the anterior capsule is intact, a standard continuous curvilinear capsulorrhexis (CCC), 5 to 6 mm in diameter, can be performed. Handle the anterior capsule gently to avoid increasing stress on the zonules. Avoid anterior capsule visualization loss, which may occur behind the iris.
Ruptured anterior capsule. A lens that becomes opacified in the course of hours or even minutes usually indicates a ruptured anterior capsule, which allows the lens fibers to become hydrated with aqueous humor.
If the CCC cannot be completed, the surgeon should cut any bridge with Vannas scissors to avoid pulling it with the phacoemulsification handpiece or irrigation and aspiration (I&A) tip.
Zonular weakness/dialysis. In this setting, the surgeon can place iris or capsular bag hooks to secure the bag for the cataract extraction. (See Figs. 4 and 5, below)
Capsular tension rings are indicated if zonular dialysis is present (30-90 degrees of zonular fibers). However, placement of a ring is contraindicated in the absence of a CCC or if posterior capsule rupture is suspected.
Cataract Extraction
Either a Venturi or peristaltic pump device may be used for phacoemulsification, depending on surgeon preference and hospital resources. The parameters should be low. (See “Clinical Pearls” for possible settings.)
Purely traumatic cataract. For a purely traumatic cataract (i.e., without a senile component), the lens nucleus can be easily aspirated with the I&A tip. It is preferable to start with the nucleus and end with the cortex; this will protect the posterior capsule from inadvertent rupture.
Alternatively, a Simcoe cannula can be used to aspirate a soft cataract. It can be introduced into the anterior chamber through an incision of 2.8 to 3.0 mm.
Combined traumatic and senile cataract. When both components are present, the hardness of the cataract should be assessed by clinical observation and factored into the surgical plan.
In our experience, we prefer to perform hydrodissection to separate the nucleus from the cortex before starting phacoemulsification. The cortex will help protect the posterior capsule.
Our preferred method for emulsifying a cataract in this setting is a divide-and-conquer technique. Stop and chop may be used if the nucleus can be visualized clearly. An Akahoshi prechopper can be used safely after a central groove has been sculpted. The surgeon must take care not to push down the nucleus during chopping maneuvers.
Clinical Pearls
 Low parameters. In the setting of trauma, phacoemulsification parameters should be conservative, for instance, using a low bottle height (60-75 cm), low aspiration rate (18-20 cc/min), and proportionally low vacuum (180-200 mm Hg). Ultrasound power varies depending on the hardness of the cataract. (Note: These parameters are presented as examples and should be adapted according to the specific phacoemulsification device and clinical scenario.) Low parameters. In the setting of trauma, phacoemulsification parameters should be conservative, for instance, using a low bottle height (60-75 cm), low aspiration rate (18-20 cc/min), and proportionally low vacuum (180-200 mm Hg). Ultrasound power varies depending on the hardness of the cataract. (Note: These parameters are presented as examples and should be adapted according to the specific phacoemulsification device and clinical scenario.)
Intracameral antibiotic. At the end of the surgery, we inject 0.3 mL of cefuroxime solution (concentration of 1.0 mg/0.1 mL) into the anterior chamber as a prophylactic antibiotic.
Hemostasis. To control bleeding during cataract extraction, dispersive viscoelastic may be used for tamponade, or intracameral epinephrine may be injected to cause vasoconstriction.
|
Complications
Vitreous prolapse. If vitreous is prolapsed in the anterior chamber, it must be removed by means of a second instrument through a lateral incision, and anterior vitrectomy should be performed (Fig. 3 and Figs. 4 and 5, below). Complications such as retinal detachment may occur if the vitreous is heated or pulled with the phaco handpiece. Vitreous should not be pulled out through the wound with a sponge.
Hyphema. If blood is present in the anterior chamber, it should be washed out and removed as soon as possible because of risk of hematocornea (corneal blood staining). During cataract extraction, bleeding may occur spontaneously. To help control bleeding, dispersive viscoelastic may be used for tamponade, or intracameral epinephrine may be injected to cause vasoconstriction.
 |
|
VITRECTOMY. Prolapsed vitreous is removed by means of bimanual anterior vitrectomy.
|
IOL Placement
The type and optimum placement of the IOL depend on the clinical context. If visualization is poor, consider placing the IOL in a later secondary procedure.
If the capsular bag is complete, a 1-piece acrylic IOL is usually placed in the bag. However, if the capsule is ruptured, a 3-piece acrylic IOL should be placed in either the capsular bag or ciliary sulcus. The latter placement is preferable if enough of the anterior capsule remains to support it. Anterior chamber lenses should be avoided in eyes with a lacerated cornea or in young patients.
 |
|
Capsular tension ring being placed after iris hooks have been used to hold open capsular bag.
|
 |
|
Dispersive viscoelastic is used to help eject vitreous from main incision.
|
Completion of Surgery
An intracameral antibiotic may be administered at the conclusion of surgery. After closure, the surgeon should assess for leakage and ensure that all wounds—whether from the initial trauma or the surgical incision—are completely sealed. If this assessment is difficult because of tissue edema, it may be helpful to gently inject air to the anterior chamber; wherever air escapes, a suture should be placed.
Postoperative management of traumatic cataract includes topical antibiotic, steroids, and a cycloplegic agent to reduce postoperative inflammation.
___________________________
1 Serna-Ojeda JC et al. Int Ophthalmol. 2015;35(4):451-458.
2 Négrel AD, Thylefors B. Ophthalmic Epidemiol. 1998;5(3):143-169.
3 Kuhn F et al. J Fr Ophtalmol. 2004;27(2):206-210.
4 Shreya MA et al. J Cataract Refract Surg. 2012;38(6):959-965.
5 Kumar A et al. Clin Experiment Ophthalmol. 2005;33(6):660-661.
___________________________
Dr. Zamora-de la Cruz is an anterior segment and cataract surgery fellow, Dr. Garzón is professor of anterior segment and cataract surgery, and Dr. Arrieta-Camacho is associate professor and chief medical officer; all are at the Instituto de Oftalmologia Fundación Conde de Valenciana, in México City. Relevant financial disclosures: None. All photographs were taken during surgeries by Humberto Matiz-Moreno, MD, associate professor and cataract surgeon at Instituto de Oftalmología Fundación Conde de Valenciana.