Download PDF
This article is part of an occasional series of MD Roundtables, in which a group of experts discuss a topic of interest in their field. This is the second part of a conversation on photophobia, led by Leah Levi, MD, of the Scripps Clinic.1 She is joined by Kathleen B. Digre, MD, of the University of Utah, and Randy H. Kardon, MD, PhD, of the University of Iowa. Following are edited excerpts from their conversation.
Diagnosis
Dr. Levi: I think most of us have had situations in which photophobia patients have a completely normal ophthalmological examination. How do you approach these individuals?
Dr. Digre: I can tell you that I have a structured approach. I first look at the history and physical examination and look for a central process. I really delve into the history—as in, when did this start, and what is their past medical history? And they absolutely should be queried about previous migraine or migraine in the family. If the history or physical exam suggests something central, then I might get neuroimaging and consider other tests. Then, at the slit lamp, I look carefully for dry eyes.
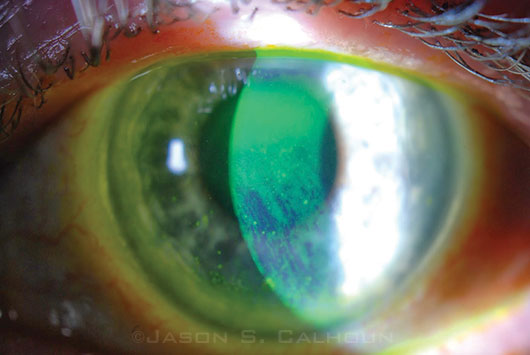
I do Schirmer testing. I look for iritis, uveitis, and corneal staining. Do they have underlying blepharitis? Do they have corneal erosion? You have to really be certain to look carefully. And sometimes I’ll apply a topical anesthetic and ask, “What effect did that have on your light sensitivity?” If that takes the sensitivity away, the condition may be localized—dry eyes or corneal neuropathy or something like that. If it doesn’t take it away, I also make sure that they aren’t actually complaining of hemeralopia or nyctalopia and have some kind of retinal problems.
Then, I look carefully at blinking—and not just what you would see in spontaneous blepharospasm but also reflexive blepharospasm when a light is shined in their eye.
Finally, migraine is so common in a lot of these people; if I’ve got migraine in the history with light sensitivity, sound sensitivity, odor sensitivity, movement sensitivity, nausea, etcetera, I’m pretty sure that migraine is participating in the cause of their photophobia. And if I don’t find anything after that, I go back to the beginning and just go through that list again. It’s either something in the history or something on the exam. It should be approached just like we do with any other ophthalmic complaint.
Dr. Kardon: I think Kathleen covered all the bases on that. It’s similar to what I go through.
 |
|
Treatment Target. Aggressive treatment of dry eye may help alleviate photophobia symptoms.
|
Treatment
Dr. Levi: When you find an ocular cause, does giving treatment directed at that underlying cause result in improvement of the symptoms—or are there some situations in which it really doesn’t?
Readaptation to Light. Dr. Digre: Well, I would like to take your case (see under “A Challenging Case,” below). As soon as these people go into the dark, you’ve got a problem, because they become dark adapted all the time. People just keep closing more shades, closing more windows, and shutting themselves off from light. They even remove LEDs from the clocks in their room. This is just going to make their condition worse. It’s as though it lowers their thresholds to the point where even the slightest light gives them pain. They really have to get back into the light, open up the shades, and start getting into brighter light, and they will adapt eventually. They should wear sunglasses outside. Just regular sunglasses are fine, even some wraparound sunglasses. They should not be wearing dark sunglasses inside.
Dr. Levi: How slowly should they do this readaptation to light? Are you talking about days or weeks?
Dr. Digre: As quickly as they can—the longer they’re in the dark, the worse it gets. They have to realize that and tolerate a little discomfort as they start getting more into the light. Then they’ll be able to tolerate more and more light as time goes on.
The real beauty of coming up with a diagnosis of photophobia is that if you can tease out the cause, then you have something you can go after. So, if they have bad dry eyes, you really need to work on that problem. If they’ve got underlying migraines, those migraines need to be treated. If they have blepharospasm, they need to have the blepharospasm treated.
Tinted Lenses and Pain Relief. Dr. Levi: Are dark glasses relatively counterproductive in your experience?
Dr. Digre: Outside, they’re appropriate. Inside, they aren’t. There are tinted lenses that do work for some people. This isn’t a panacea, but the one we have been using is called FL-41 tint. This was first mentioned 30 or 40 years ago by a group in England, and it was formulated for people with fluorescent light sensitivity. It seems to block certain wavelengths of light—around 480 nanometers—and for some people, it is very helpful.
I’ve had some luck treating some of the pain associated with photophobia. Amitriptyline treats migraine; it’s a very good medication, even at low doses. I’ve also had some luck with gabapentin for pain. And then there’s onabotulinum toxin [Botox]; we’ve seen it help several people whose main complaint is photophobia.
Dr. Levi: Randy, you mentioned blue-blocking glasses with orange tint.1 Is that more effective than the FL-41 tint? How do you advise patients on which tint they might want to use?
Dr. Kardon: Well, the blue-blocking lens is the same one Kathleen mentioned. Some patients have access to lenses that are found in sporting goods stores. Hunters use them; they’re orange. These are similar to, I believe, what she has been using. There are small differences [between the lenses], but they’re worth trying. As she indicated, it provides some relief to some patients. It’s not a universal treatment effect that patients are always satisfied with, but every little bit helps.
Novel Contact Lens. Dr. Kardon: [Researchers from] Syracuse reported at ARVO 2 years ago that they were using the soft contact lenses with an artificial pupil where the back of the iris is opaque, not just tinted.3 These were developed for aniridia patients, and there’s a 4-millimeter opening in the contact lens that limits peripheral light coming in. The downside is that it does obstruct some peripheral vision, but the group of patients they tested experienced a significant amount of relief from wearing those lenses. So that’s another potential option. I haven’t tried them in very many patients yet.
Pilocarpine. Dr. Levi: Have you tried pilocarpine drops with patients with the same kind of thing in mind?
Dr. Kardon: This same group tried pilocarpine drops, which had some effect but not as much as a contact lens. As I noted earlier,1 if you have a lightly pigmented iris, even constricting the pupil pharmacologically to a miotic state doesn’t adequately limit the amount of light getting to the retina.
Migraine Prophylaxis. Dr. Levi: Kathleen, you mentioned migraine medication. Now, for those patients who are not actually getting migraine headaches currently but have chronic photophobia, are medications used for migraine prophylaxis effective?
Dr. Digre: Some of them. In posttraumatic photophobia patients, the anti-migraine drugs might be helpful, and Botox may also be helpful.
Dr. Levi: What are the most helpful migraine prophylactic medications for photophobia? You’ve already mentioned amitriptyline and gabapentin. Are any others effective?
Dr. Digre: All of the migraine medications might be effective. We have no way of knowing which one is best for each individual.
Treating Anxiety. Dr. Digre: I do want to mention that we have found that some people with chronic photophobia also can have underlying depression and anxiety—especially anxiety. And treating that, if they have it, is also really helpful.
Dr. Levi: That’s a good point because often migraine has a stress trigger, and I’m sure that being anxious and depressed about the symptoms doesn’t really help.
Dr. Digre: Both anxiety and depression have a physiologic basis in the brain, and this may contribute [to photophobia]—and it’s been shown sometimes in laboratory animals that stress exaggerates painful responses.
CGRP Research. Dr. Levi: Again, on the migraine issue: Randy, you had mentioned calcitonin gene–related peptide (CGRP).1 Are any medications antagonistic to that available?
Dr. Kardon: Not yet. There were some phase 3 trials of antagonists of CGRP, but because of some liver toxicity in a small number of patients, that drug development has stopped. Some companies are developing antibodies to CGRP that are injected. The idea is that this could last for more than a few weeks, and it might somehow modify the CGRP-mediated migraine and possibly photosensitivity, but this is not yet available for clinical use.
Superior Sympathetic Blocks. Dr. Levi: Kathleen, you’ve also published about people who have severe photosensitivity and pain syndrome. I’m sure that this isn’t very common, but [you cited cases] where a superior cervical ganglion block has been effective.2 Is that applicable to people who have extreme photophobia and nothing has really alleviated it?
Dr. Digre: Many of the cases we had looked like complex regional pain syndrome. They had an injury to their cornea, and the injury healed, but they developed this kind of reverberating circuit of light sensitivity to just normal light. And then we did some superior sympathetic blocks with an anesthesiologist, they had relief of this symptom. So, I put this in my armamentarium. It’s a little bit more invasive, so it’s not my first-line, go-to treatment, but I think when people have a history of some kind of injury or corneal injury, maybe [they develop] reflex blepharospasm with this injury or they haven’t responded to less-invasive treatments, I think that the cervical sympathetic block definitely can be offered. We still do it in certain cases.
Dr. Levi: I’m sure that this is a very uncommon situation, but I’m sure there are ophthalmologists out there where this has happened to one of their patients after even routine cataract surgery or LASIK.
Dr. Digre: That’s right.
A Challenging Case
Dr. Levi: Back to my patient. She was truly a challenge. She has dry eye. She has convergence insufficiency, which is in turn a partial trigger for her migraines. She has extreme light sensitivity. She is more tolerant of lights now that she’s on migraine prophylaxis, but she still has problems with computer screens to the extent that she can’t even do her convergence exercises, which are computer-based.
At this point, what suggestions would you have?
Dr. Digre: I would start with some pencil push-ups and not use the computer for convergence exercises, as it’s a trigger from the light point of view. I think trying an FL-41 or a similar type of lens might be helpful. There are Internet sources for these lenses, but make sure that the lens blocks the blue-light spectrum. Sometimes the makers say they do, but they really don’t. I’d maximally treat the dry eyes, maybe with lubrication at night and tears during the day, and then I’d work on migraine prevention. I’d push up the migraine prevention so that the headache portion of this is completely under control.
Dr. Kardon: I would try to find out if the convergence insufficiency is really part of the syndrome. Usually, I do that by having them patch one eye to verify whether it improves their symptoms. In addition, if the patient does have dry eyes, I have a low threshold for putting in punctal plugs, since it’s a pretty benign procedure. A lot of patients just don’t put in enough drops during the day to make a difference, and I think silicone punctal plugs are a pretty easy way of really trying to mitigate that part of the equation.
Dr. Digre: I totally agree.
They Aren’t Crazy
Dr. Levi: Do either of you have any final comments?
Dr. Digre: I would just like to say that ophthalmologists need to own photophobia as an eye complaint. This is a problem that we all need to be able to evaluate and treat, and we can’t just say, “Oh, well, I don’t see anything wrong. It’s not your eyes; see somebody else.” I think that’s where people like your patient are just going in circles, seeing one doctor after another. An ophthalmologist may want to partner with a neurologist or a headache specialist to try to get the headache component under control, but we ophthalmologists really need to first own this symptom as real, then come up with the right diagnosis, and then suggest plausible treatment.
Dr. Kardon: I couldn’t agree more.
Dr. Digre: To refer back to your patient, that’s exactly the kind of patient I get sent all the time. Nobody’s taking them seriously.
Dr. Levi: A lot of these patients are just blown off as being “crazy.” And pain and photophobia actually can make you a bit desperate.
Dr. Digre: And the anxiety is probably part of the pathophysiology. I didn’t want to get into the animal studies, but there’s one done by Andrew Ahn and his colleagues in newborn rodents. Newborn rodents don’t have vision, but they do have active melanopsin cells, so they can sense light. These animals were put into light, and they started squealing just like they do when they are taken away from their mother. It is an anxiety response. Then the researchers looked at the brains of these animals and saw that the amygdala and several of the emotional centers were triggered.4 If animals can have stress and anxiety related to light, this is a real deal. This anxiety component is an important one.
___________________________
1 See “MD Roundtable: Solving the Photophobia Puzzle” in the November 2015 issue.
2 Fine PG, Digre KB. J Neuroophthalmol. 1995;15(2):90-94.
3 Jackowiski MM, Motter B. Poster 5307-D0068 presented at: Association for Research in Vision and Ophthalmology Annual Meeting; May 8, 2013; Seattle.
4 Delwig A et al. PLoS One. 2012;7(9):e43787. doi:10.1371/journal.pone.0043787.
___________________________
Dr. Digre is professor of ophthalmology and visual sciences and neurology at the John A. Moran Eye Center at the University of Utah in Salt Lake City. Relevant financial disclosures: Is a coinventor, with a patent pending, on a lens technology; she received less than $100, which was given to the ophthalmology department at Moran Eye Center.
Dr. Kardon is professor of ophthalmology and visual sciences and director of the Neuro-ophthalmology Service at the University of Iowa in Iowa City. Relevant financial disclosures: Department of Defense TATRC: S; MedFace: O; National Eye Institute: S; Novartis: C; Veterans Administration: S.
Dr. Levi is director of neuro-ophthalmology at Scripps Clinic in La Jolla, Calif. Relevant financial disclosures: None.
See the disclosure key at www.aao.org/eyenet/disclosures.