By Julia A. Haller, MD, with Diana V. Do, MD, and Peter K. Kaiser, MD
Download PDF
In last month’s EyeNet, Julia A. Haller, MD, of Wills Eye Hospital, hosted a roundtable discussion on anti–vascular endothelial growth factor (anti-VEGF) therapy for age-related macular degeneration (AMD). In this second installment, Dr. Haller continues her conversation with Diana V. Do, MD, of the University of Nebraska, and Peter K. Kaiser, MD, of the Cleveland Clinic Cole Eye Institute. The trio share thoughts on important considerations for managing patients with AMD, including systemic concerns, ocular comorbidities, genetic testing, and home monitoring.
Systemic Considerations
Dr. Haller: There is some debate in the literature about the possible systemic effects of anti-VEGF therapy. Are systemic concerns part of your equation with these drugs?
Dr. Kaiser: I ask patients if they’ve had a recent [within the last 5 years] arterial thrombotic event such as a stroke or heart attack. We know from many studies that anti-VEGF treatment in these patients may increase the risk of another arterial thrombotic event. In these patients, I try to reduce the treatment frequency as much as I can. If the patient has a type 1 choroidal neovascularization [sub-RPE vascular proliferation], I would obtain an indocyanine green angiogram to evaluate for polypoidal choroidal vasculopathy, where the addition of photodynamic therapy can be considered. Several studies have shown that by adding photodynamic therapy, we don’t improve efficacy but can reduce the number of injections. In other types of CNV, we need to continue anti-VEGF injections. A very frank discussion with the patient about the risks and benefits of therapy is needed. I explain that the risk of another stroke is roughly 10% if anti-VEGF treatment is continued—but that there is almost a 100% certainty that there would be some loss of vision if the treatments are stopped. With knowledge of the risks and benefits, the patient is able to make an informed decision about continuing treatment.
With respect to overall arterial thrombotic events, numerous comparison studies have shown that the safety profiles are reasonably similar between bevacizumab, ranibizumab, and aflibercept.
Dr. Do: In a recent Cochrane systematic review of patients with AMD,1 the systemic safety of bevacizumab and ranibizumab was evaluated. The researchers could not determine a difference between intravitreal bevacizumab and ranibizumab for rates of arterial thrombotic events and deaths through 2 years of treatment. If a difference exists between these agents, it is likely to be small and will be difficult to determine because retina clinical trials are not powered to detect very small differences in uncommon adverse events.
If one looks at all the safety data for ranibizumab, bevacizumab, and aflibercept, there is no clear-cut evidence to suggest that any of these agents has a detrimental effect on systemic health. For the vast majority of my patients, even those with cardiovascular or systemic risk factors, I still recommend intravitreal treatment if they need it to save their vision. For example, the biggest risk factor for a second stroke is the patient’s medical history of prior cerebrovascular events.
Dr. Haller: So you wouldn’t select one anti-VEGF agent over another based on systemic absorption, because you regard them all as equally safe?
Dr. Do: Correct. I think ranibizumab, bevacizumab, and aflibercept are all relatively safe treatment options, and there is no clear evidence to suggest that any particular agent has superior systemic safety.
Dr. Kaiser: I agree, although you could potentially reduce injection frequency by using aflibercept. If I have a patient on bevacizumab who has had a recent stroke or heart attack, I will switch them to aflibercept, not because I’m worried about the drug itself but to reduce the number of injections.
Genetic Testing and AREDS Supplements
Dr. Haller: Patients have read about genetic testing, and we’re telling them that the major risk factor for AMD is genetic predilection. Are you advising genetic testing, and are you recommending AREDS2 supplements?
Dr. Kaiser: In patients with dry AMD, one could consider genetic testing, but the evidence is currently weak that doing this will change outcomes over what we currently recommend for these patients—AREDS2 vitamin supplementation and a good diet. Once wet AMD develops, I think that genetic testing is not advisable. There has been some suggestion that certain genetic subtypes respond differently to anti-VEGF medications, but the evidence for that is rather weak, and the results of genetic testing in a patient with wet AMD wouldn’t change my management of the patient.
If the patient has wet AMD in one eye and dry AMD in the other, then yes, AREDS2 supplementation is certainly worthwhile to reduce the risk of AMD progression in the dry AMD eye. However, we know that supplementation won’t necessarily reduce the risk of progression in the eye with wet AMD. If the patient has wet AMD in both eyes, then I would let the patient decide; we don’t know whether AREDS2 supplementation will help.
Dr. Do: I agree on recommending the AREDS2 supplementation, and I also counsel patients on additional lifestyle modifications. If the patient is an active smoker, I strongly recommend smoking cessation because smoking has been shown to increase the risk of AMD in numerous population-based studies. Results of the AREDS2 trials also indicate that we could use lutein and zeaxanthin in place of beta-carotene for reducing the risk of progression to advanced AMD. In addition, using the AREDS2 formulation with lutein and zeaxanthin is important because beta-carotene supplementation has been associated with an increased risk of lung cancer in patients who were prior smokers.
Currently, I do not think there’s a clear role for genetic testing in AMD patients. In addition, genetic testing is not covered by Medicare or most insurance carriers, and it can be a financial burden for patients who pay for it out of pocket. [Editor’s note: The Academy clinical statement, Recommendations for Genetic Testing of Inherited Eye Diseases, is available online.]
Glaucoma and Cataract
Dr. Haller: Is there any ocular condition, such as glaucoma or cataract, that would influence your treatment decision?
Dr. Kaiser: Repeated intravitreal injections, regardless of the drug, can lead to elevated intraocular pressure in some patients. This is something to watch for. In addition, a few studies have suggested that prolonged anti-VEGF use can affect the nerve fiber layer. Reducing the number of injections is a goal for every patient, but especially for patients with glaucoma.
Cataract surgery in the context of AMD is a common scenario. I recommend performing cataract surgery in a patient with AMD when they need it, just as you would for a patient without AMD. I wouldn’t push for cataract surgery until the patient really needs it, but I am not afraid to recommend cataract surgery in the setting of exudative AMD.
There have been some suggestions that a patient with AMD who is well treated and well managed could experience relapse of wet AMD after cataract surgery. Rather than attributing an explosion of AMD to the surgery, I think it’s more likely that the patient may have missed some postoperative follow-up with the retina specialist. Therefore, I am very proactive about working with the cataract specialist. I want to make sure that the cataract extraction is done at approximately the same time that I would have performed a treatment injection. I ask the cataract specialist to administer an injection right after surgical closure so that the patient receives a full dose of the anti-VEGF agent at that time. This avoids a missed AMD treatment during the early postoperative period. We have many cataract surgeons who operate at the Cleveland Clinic, and we routinely give anti-VEGF injections in the operating room at the end of the cataract procedures.
Dr. Haller: So if you were following the treat-and-extend regimen, and it had been 2 months since the last injection, you would still feel comfortable with the patient receiving cataract surgery, as long as the retina was dry and the patient would receive an injection at the time of surgery?
Dr. Kaiser: Exactly.
Dr. Do: I think that cataract surgery in patients with underlying AMD is a safe option, and the AREDS trial showed that cataract surgery can result in improved vision without an adverse ocular outcome. If a patient has a mature cataract and needs cataract surgery, I would allow them to undergo surgery; I would then monitor the AMD closely and treat the eye as needed with an intravitreal VEGF blocker if there is active choroidal neovascularization.
Dr. Haller: I think it is important for the retina to be as dry as possible going into the slight stress and trauma of surgery, even in the hands of our top cataract experts. This operation is on a very delicate organ. I usually administer anti-VEGF treatment the week before the cataract operation, even if normally I wouldn’t have treated the patient for another month or so. I like to top the patient off before cataract surgery or before a glaucoma operation such as trabeculectomy.
Home Monitoring
Dr. Haller: Are there any new types of monitoring that you’re recommending? Are you giving patients an Amsler grid, or are you figuring that you’re going to see them back so soon that they don’t need to monitor at home?
Dr. Do: I see many of my patients with active neovascular AMD almost every month, and I think that my clinical exam and the optical coherence tomography scan at follow-up are providing a high level of monitoring for their fellow eye.
For patients with intermediate AMD, typical follow-up is every 6 months, and I advise them to monitor at home either by covering each eye separately and using the Amsler grid or by employing home monitoring devices such as ForeseeHome [Notal Vision]. Home monitoring with new devices can be useful for some patients, but not all patients have the cognitive or physical ability to do such monitoring.
Dr. Kaiser: Home monitoring is a very exciting field that is just starting to be explored. I ran a study for Novartis a couple years ago, looking at the use of an iPhone-based app for home monitoring.2 That study was the basis for FDA approval of this app [myVisionTrack, Vital Art and Science]. The ForeseeHome device also has been FDA approved for home monitoring, and we’re seeing the advent of numerous iPhone-based visual testing applications. Many of my patients use an app called Paxos Checkup from DigiSight Technologies. I don’t recommend home monitoring to all of my patients, but I have many patients who want to be more proactive, especially if we’re doing an as-needed treatment regimen (which I generally avoid), so I would recommend home monitoring for them.
We learned from the Novartis study that elderly patients could perform a daily visual test on an iPhone. We had specifically enrolled elderly patients [the majority of whom were 75 years or older] in that study, including many who did not own an iPhone and did not consider themselves savvy technologically. These patients did great; we administered a survey before and after the study, and almost 95% of all patients felt very comfortable with this application and had no problems performing the visual test on the iPhone.
Dr. Haller: The ForeseeHome system also was found to work very well in the AREDS2 study. My experience has been that some ocular changes are challenging to interpret from a home-based device, and you will have to see the patient. Detecting a conversion from dry to wet is not always straightforward. For example, I have a patient who is about 65 years old, which is relatively young for AMD. She has pigment epithelial detachments in both eyes and gets small shifts on her cloud-based monitoring, and I’m not sure exactly what’s going on without a clinical exam.
Dr. Do: I agree that sometimes it is challenging to interpret results of home monitoring, and it’s always safer to have the patient come in for clinical evaluation to determine whether there’s been conversion to wet AMD.
Dr. Kaiser: I caution patients not to rely 100% on home monitoring. If they think they are experiencing a change, even if the device is not registering a change, I encourage them to be evaluated.
Dr. Haller: There’s a lot of interesting work being done with home monitoring for AMD. I think it’s a very exciting new player in the field that hopefully will be very helpful as we’re caring for a growing population of patients with AMD.
___________________________
For more information about home monitoring, see “Catching CNV Early With At-Home Monitoring” in the September EyeNet.
___________________________
Listen to the roundtable below:
___________________________
1 Moja L et al. Cochrane Database Syst Rev. 2014;9:CD011230. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD011230.pub2/full. Accessed Sept. 16, 2016.
2 Kaiser PK et al. Retina. 2013;33(9):1863-1870.
___________________________
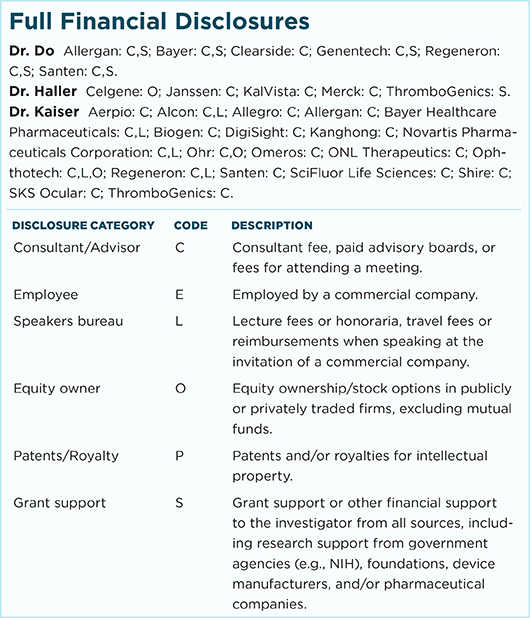
Dr. Do is a professor of ophthalmology and vice chair for education at the University of Nebraska Medical Center in Omaha. Relevant financial disclosures: Allergan: C,S; Bayer: C,S; Genentech: C,S; Regeneron: C,S.
Dr. Haller is Ophthalmologist-in-Chief at Wills Eye Hospital in Philadelphia. Relevant financial disclosures: Celgene: O; Janssen: C; KalVista: C; Merck: C; ThromboGenics: S.
Dr. Kaiser is the Chaney Family Endowed Chair for Ophthalmology Research and a professor of ophthalmology at the Cleveland Clinic Lerner College of Medicine in Cleveland, Ohio. Relevant financial disclosures: Alcon: C; Allergan: C; Bayer: C; DigiSight: C; Kanghong: C; Ohr: C; Ophthotech: C; Regeneron: C; SKS Ocular: C, S.
For full disclosures and the disclosure key, see below.