By David A. Plager, MD, with Fiona E. Costello, MD, and Sharon F. Freedman, MD
Download PDF
Last month’s issue of EyeNet contained part 1 of a roundtable discussion hosted by David A. Plager, MD, of Indiana University and Riley Hospital for Children. In this second installment of the 2-part series on optical coherence tomography (OCT) in pediatric patients, Dr. Plager resumes his conversation with Sharon F. Freedman, MD, of Duke University Eye Center, and Fiona E. Costello, MD, FRCPC, of the University of Calgary. The experts offer insight on incorporating OCT into the longitudinal evaluation of children with optic neuropathy.
Pediatric Glaucoma
Dr. Plager: How do you apply OCT alongside traditional metrics for following glaucoma in children?
Dr. Freedman: It depends on the patient. A child may be referred to me with suspected glaucoma based on visual inspection of the optic nerve, and I would use OCT to examine the amount of rim tissue in the optic nerve head via measurement of the retinal nerve fiber layer and macular thickness maps. The patient may have a large optic nerve head with a large cup and a healthy rim; in that case, a completely normal and symmetrical RNFL in both eyes would provide reassurance, along with normal eye pressures, that the cupping is physiologic. Conversely, a second patient may have a much smaller nerve with a small cup, but OCT may confirm a thin RNFL, suggesting an optic nerve damage not so easily seen on clinical examination alone.
We still lack a truly normative database of OCT values in children, and even if we had one, the range of “normal” is quite large across children of varying ages, ethnicities, and axial lengths. Nevertheless, OCT is very helpful for assessing a child with presump tive glaucoma but normal intraocular pressure (IOP) who is considered low risk. For such a patient, the central corneal thickness should be determined to be sure it is not abnormally thin, and the family history should be reviewed for early onset glaucoma. If the patient’s parents are present, I may examine the sizes of their optic nerves and cups for comparison. In the pre-OCT days, if all these features were normal, and results of the workup otherwise were normal, I would simply monitor the patient for elevated intraocular pressure. However, being able to measure the RNFL and macular thickness, and finding the values robust and symmetric, give me much more confidence that the nerve is healthy and the cup is nonglaucomatous. OCT findings also provide a good baseline for longitudinal monitoring. If the patient’s OCT results are unchanged through 1 year of follow-up, with no other features worrisome for glaucoma such as elevated intraocular pressure, I would consider the risk of glaucoma to be very low.
As an alternative example, a child with 20/20 visual acuity and no ophthalmic concerns may undergo testing at an optometrist’s office and have abnormal OCT results. The scan may show an optic nerve pit or a region of the optic nerve that appears underdeveloped, and this may be accompanied by a matching visual field defect. In such cases, visual inspection of the nerve can yield crucial information; for example, it may show that the abnormality likely does not result from a progressive disease process but rather is a nonglaucomatous congenital defect of the optic nerve.
Dr. Costello: I have identified more cases of optic nerves with segmental hypoplasia by OCT than by visual examination. OCT enables detection of subtle differences in symmetry that may be missed by clinical evaluation alone.
Dr. Freedman: Consider a child who was born prematurely and has an associated morbidity of the central nervous system (CNS), such as interventricular hemorrhage, periventricular leukomalacia, and/or mild cerebral palsy. On examination, the patient has large optic nerve cups with borderline elevated IOP, and OCT findings show very low RNFL thickness in both eyes. My recommendations would be to consider that OCT result as the baseline, presume that the RNFL thickness is low because of trans-synaptic CNS damage associated with prematurity, and suggest longitudinal monitoring.
Dr. Costello: I agree regarding the value of longitudinal follow-up. When asked to assess a patient with an acquired optic neuropathy, I often say, “I have a snapshot, and I need a movie. Therefore, I need to collect more data points over time.”
True Change
Dr. Plager: How much change in successive OCT results do you expect to see before you regard an effect as real and not just fluctuations between scans?
Dr. Costello: In my experience, the test-retest variability for an OCT machine is generally 5 to 6 μm.
Dr. Freedman: I agree.
Dr. Costello: When I start to see changes in overall (mean) peripapillary RNFL measurements in excess of 5 to 6 μm—and certainly in excess of 10 μm—I would suspect pathology. I might be looking at subtle optic disc edema or subtle manifestations of atrophy.
Dr. Freedman: OCT is particularly helpful in early glaucoma because a patient may lose up to 60% or 70% of the RNFL and still be preperimetric.1,2 These data come mostly from adults but likely are true for children as well.
If you require presence of a visual field defect to confirm that glaucoma is progressing, much of the RNFL will be lost before you get a positive result. In preperimetric or early perimetric stages of glaucoma, serial OCT scans are invaluable for monitoring progression.
As the RNFL gradually is damaged and diminished—such as to a thickness of 43 μm that decreases to 41 or 38 μm by the next visit—this layer becomes too thin to monitor change reliably with OCT. At that point, visual field testing should be your preferred mode of monitoring, assuming the patient is cooperative. In my experience, patients who are at least 6 years old and cognitively normal, and who have relatively good central visual acuity and no nystagmus, can usually maintain the fixation necessary for OCT analysis, whereas many 10-year-old patients still are unable to undergo reliable visual field testing.
I agree that a global RNFL change of more than 6 or 7 μm is concerning and likely indicative of true change. However, for pediatric patients, you have to be particularly attentive to the tracing on the OCT output. I have obtained OCT results that are phase shifted from the patient’s previous results, which suggested that the child moved during testing, not that the RNFL had thinned. In contrast, global thinning of the RNFL—involving, for instance, the superotemporal and inferonasal sectors—is more worrisome. As with visual field testing, the findings of repeated OCT studies are helpful for identifying change.
Dr. Costello: In follow-up for patients with a CNS demyelinating process, such as multiple sclerosis, I look for subclinical manifestations of damage to the afferent visual pathway, including sectoral or global RNFL thinning and ganglion layer loss. In general, you should obtain a high-quality scan, have a good understanding of the disease that you’re following, and confirm that the results are reproducible so that you know the OCT findings are real rather than artifactual.
Dr. Freedman: There also are cases in which results of RNFL thickness do not give a complete picture. For example, a uveitic eye can have subtle macular thickening and can resemble papilledema with atrophy. In Sturge-Weber syndrome, a very thick choroid can preclude or make more difficult good OCT measurements of the RNFL.
Dr. Costello: I agree. For a patient with a compressive etiology, such as pituitary adenoma, results of ganglion layer analysis may show nasal hemiretinal thinning in advance of the bitemporal hemianopsia that hasn’t manifested yet (but will over time).
With OCT, you can evaluate patterns beyond those of the peripapillary RNFL to understand pathologies involving the optic nerve, the chiasm, or the tract. Some patients may even have retrogeniculate causes of vision loss, such as tumors, that can induce retrograde trans-synaptic degeneration. This degeneration yields a specific pattern of ganglion layer loss in OCT analysis that correlates with the visual field deficit. For OCT findings to be meaningful and interpretable, you need at least a fundamental understanding of the disease you’re following.
In adult patients with dominant optic atrophy, OCT may show extreme thinning of the peripapillary RNFL and ganglion layer measures, but visual function by standard automated perimetry may be better than expected, possibly because of cortical adaptation. These findings (a dissociation between structure and function) may suggest a chronic process acquired in early childhood, rather than an acute ischemic or inflammatory condition acquired in adulthood.
Dr. Freedman: Resilience of the optic nerve varies among children with high IOP. One patient showed an unusual and asymmetric progression of optic nerve cupping and corresponding RNFL loss in the right eye over less than 2 years when his pressures rose in both eyes. In contrast, a patient with aphakia and a small optic nerve can have pressure ranging from 20 to 30 mm Hg for a very long time and still maintain normal RNFL thickness.
For pediatric patients with glaucoma who can undergo OCT, this technology gives us a way to detect subtle disease progression even when the IOP is within the target range. We can identify and treat structural loss, hopefully before the patient experiences a visual field defect. Conversely, for a patient with pressure in the low 20s, longitudinal OCT findings confirming a stable RNFL and hence a healthy optic nerve are reassuring.
Dr. Costello: For pediatric patients with suspected functional (nonorganic) vision loss, normal OCT measures obtained repeatedly over time can provide reassurance that afferent visual pathway structure is preserved. In cases of optic neuritis, OCT measures change over time, often showing progressive peripapillary RNFL thinning and ganglion layer loss. For conditions that mimic optic neuropathy, such as acquired retinal disorders in which there is a substantial visual field defect and a normal-appearing optic nerve, I would recommend OCT testing and/or electroretinography. You should consider other mechanisms for vision loss than chronic optic neuropathy in the setting of normal peripapillary RNFL and ganglion layer measures.
Dr. Freedman: Our discussion has focused on the inner retina, which is what Dr. Costello and I see often, but there are times in a pediatric ophthalmology practice when you cannot get a patient’s refraction where it needs to be—maybe the patient’s optometrist or pediatrician couldn’t either—and you have to decide if there is a functional defect. I don’t necessarily trust only my opinion in such cases. I have had several patients whose OCT findings indicated early Stargardt disease, disruption of the ellipsoid zone, or early photoreceptor loss. These children unfortunately may languish as malingerers when they actually have outer retinal changes. Once we’ve differentiated functional deficits from real retinal problems, we can refer these patients to our retina colleagues and other support services for low vision.
Dr. Costello: That’s an excellent point. Without OCT, we’re often waiting for more glaring changes to emerge in results of qualitative assessments of the optic nerve. Thus, we may miss subtle preclinical manifestations of an acquired optic neuropathy. As a result, the patient’s diagnosis can be delayed.
Imaging Frequency
Dr. Plager: For a case that seems relatively stable, such as optic neuropathy or glaucoma with borderline abnormal IOP that is being managed with eyedrops, how often do you repeat OCT before you expect that you might see some change?
Dr. Freedman: Generally, glaucoma patients in my practice undergo annual OCT testing. For some patients, I want to avoid surgery, whereas other patients have undergone surgical procedures already and we really need to know if the disease is worsening. If I see a change in imaging findings compared with the previous year or if I’m having trouble establishing whether the patient’s condition is stable or warrants intervention, I will repeat OCT as frequently as every 4 months.
For high-pressure glaucoma, especially severe juvenile open-angle glaucoma, in which the RNFL has thinned to approximately 40 to 50 μm, I’ll perform a procedure to decrease the intraocular pressure, and the nerve may reverse the cupping, but the RNFL will continue to thin for a bit. This phenomenon may be due to damaged and perhaps even swollen nerve fibers that continue to undergo apoptosis after the procedure, despite the pressure being lower. Unfortunately, even if you lower IOP in patients with glaucoma, damage to the RNFL does not improve.3
Dr. Costello: I agree. In cases like compressive optic neuropathy, I’ve seen progressive loss of the ganglion layer and sometimes the RNFL, even after the source of compression is removed. I think the continued loss corresponds to vulnerable axons and neurons that already were committed to a process of damage or loss, despite removal of the insult.
I can provide 3 examples of how I use OCT to monitor patients with ophthalmic conditions other than glaucoma and how I interpret changes in longitudinal results. My approach to OCT is practical.
For a patient with idiopathic intracranial hypertension, I would use results of perimetry, fundus examinations, and OCT to demonstrate beneficial effects of treatment over a series of clinic visits. If the patient has started treatment with acetazolamide, repeat OCT testing (over intervals of weeks to months) will show gradual improvement in optic nerve swelling and normalization of the peripapillary RNFL. OCT results, in conjunction with functional outcomes, guide my decision-making for tapering or increasing their medication. Rather than simply telling the patient and parents that there is Frisén grade 2 or 3 swelling of the optic nerve, I’m able to show them the structural findings over time, in a meaningful way. Moreover, I can detect subtle increases in RNFL thickness in patients with less well-controlled idiopathic intracranial hypertension, versus stability (in RNFL measurements) in patients with good disease control.
For a pediatric patient with multiple sclerosis, loss of peripapillary RNFL or ganglion layer thickness in the absence of a discrete (clinically overt) optic neuritis event is concerning because it suggests that subclinical disease activity is not being controlled sufficiently by the patient’s disease-modifying therapy. In such a case, I would talk with my pediatric neurology colleague about therapeutic strategies, which may improve the patient’s disease control.
For a patient with buried optic disc drusen, I would use serial OCT testing to monitor drusen size and location (superficial versus buried). In the setting of superficial optic disc drusen, I would look for evidence of subtle changes over time in the integrity of the peripapillary RNFL and the ganglion layer that might correlate with evolving visual field defects.
Use of OCT and interpretation of the results should be driven by context. To determine if a patient’s condition is improving, worsening, or staying the same on the basis of OCT findings, you must have an understanding of the disease process and its underlying cause. Only then can you separate signal from noise.
___________________________
Listen to the roundtable below:
Download Audio
___________________________
1 Zangwill LM et al. Arch Ophthalmol. 2005;123(9):1188-1197.
2 Dong ZM et al. Invest Ophthalmol Vis Sci. 2016;57(9):OCT556-567. doi:10.1167/iovs.16-19933.
3 Ely AL et al. Am J Ophthalmol. 2014;158(5):905-915.
___________________________
Dr. Costello is Associate Professor in the Departments of Surgery and Clinical Neurosciences at the University of Calgary in Alberta. Relevant financial disclosures: None.
Dr. Freedman is Chief of Pediatric Ophthalmology and Professor of Ophthalmology and Pediatrics at Duke University Eye Center in Durham, N.C. Relevant financial disclosures: None.
Dr. Plager is Professor of Ophthalmology at Indiana University School of Medicine and a pediatric ophthalmologist at Riley Hospital for Children in Indianapolis. Relevant financial disclosures: None.
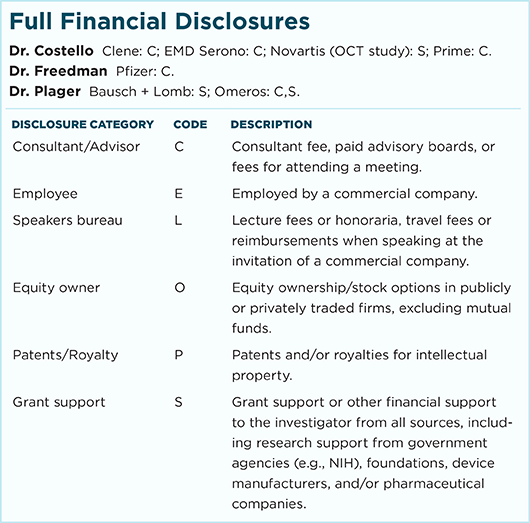
For full disclosures and the disclosure key, see below.