This content is excerpted from EyeNet’s MIPS 2020; also see the Academy’s MIPS hub page.
Based on your 2020 MIPS final score, CMS will apply a payment adjustment to your 2022 Medicare Part B payments.
CMS continues to raise the bar. To avoid a payment penalty in 2022, you need a 2020 MIPS final score of at least 45 points (up from 30 points in 2019); to earn an exceptional performance bonus, you need to score at least 85 points (up from 75 points in 2019).
Table: Bonuses and Penalties
| 2020 MIPS Final Score |
2022 Payment Adjustment |
| 0-11.25 points |
Maximum penalty of –9% |
| 11.26-44.49 points |
Penalty on a sliding scale (see table below) |
| 45 points |
Neutral (no penalty, no bonus) |
| 45.01-84.99 points |
Initial bonus* |
| 85-100 points |
Initial bonus* + exceptional performance bonus† |
|
* The initial bonus is based on a linear sliding scale—those who score 45.01 points get the lowest bonus; those who score 100 points get the highest.
† The exceptional performance bonus is based on a linear sliding scale—those who score 85 points get the lowest bonus; those who score 100 points get the highest.
|
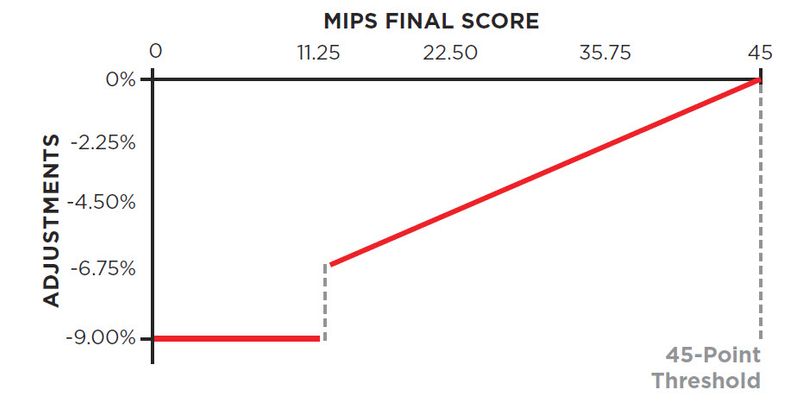
Potential penalties are higher. The maximum payment penalty has increased to –9% (up from –7% for the 2019 performance year/2021 payment year).
Table: Payment Penalty
If your 2020 MIPS final score is less that the 45-point performance threshold, your 2022 Medicare Part B payments will be reduced as shown below.
 Although CMS has set the negative payment adjustment (as shown above), it doesn’t yet know what the positive payment adjustments will be.
Although CMS has set the negative payment adjustment (as shown above), it doesn’t yet know what the positive payment adjustments will be. The bonus for scoring more than 45 points (the initial bonus) will be funded by payment penalties. Consequently, CMS won’t be able to estimate how much money is in the bonus pool—and how many clinicians will be entitled to money from that pool—until it has calculated the MIPS final scores of all MIPS participants, which can’t happen until the performance year is over. Similarly, until CMS knows how many MIPS eligible clinicians have scored at least 85 points, it won’t know how far it has to stretch the $500-millon bonus pool for exceptional performance.
Why is there a gap year between performance (2020) and payment adjustments (2022)? CMS needs time to process the MIPS data, determine final scores, perform targeted reviews, and calculate an adjustment factor that ensures budget neutrality.
How the Bonuses and Penalties Will Be Applied
You can report and be scored as an individual and/or as part of a group. If you are scored as an individual, CMS will use both your Tax Identification Number (TIN) and National Provider Identifier (NPI) to distinguish you as a unique MIPS participant. If you and your colleagues report as a group, the group’s TIN will be used as your identifier for scoring purposes. You also can report both ways and see which approach scores higher (see “Participate as an Individual or as a Group?”).
Payment adjustments are always applied at the TIN/NPI level. CMS will apply the payment adjustments at the TIN/NPI level, regardless of whether you were assigned a MIPS final score as an individual or as part of a MIPS group.
Your 2020 final score will follow you to your next practice. Your 2020 final score will determine your 2022 payment adjustment, and this is the case even if you move to a new practice after the 2020 performance year is over.
The payment adjustments will be applied throughout the year. CMS will start applying the MIPS payment adjustments in 2022. They will be applied throughout the year to your Medicare Part B remittances.
Table: How the Bonuses Are Funded
|
2020 MIPS Final Score
|
2022 Payment Adjustment
|
|
Provenance of Bonus Dollars
|
|
0-11.25 points
|
–9% penalty (negative payment adjustment)
|
→
|
The negative payment adjustments reduce CMS expenditure. These savings go into a bonus pool that funds the initial bonuses (which are therefore budget neutral).
These initial bonuses are paid on a linear sliding scale. (Those who score 45.01 points get the lowest bonus, those who score 100 points get the highest.)
|
|
11.26-44.99 points
|
Payment penalty on a linear sliding scale, as shown in Table 15 (negative payment adjustment)
|
→
|
|
45 points
|
Neutral (no payment adjustment)
|
|
|
45.01-84.99 points
|
Initial bonus (payment adjustment)
|
←
|
|
85-100 points
|
Initial bonus (payment adjustment)
|
←
|
|
+ exceptional performance bonus (additional payment adjustment)
|
←
|
Funded by a separate $500-million bonus pool, these exceptional performance bonuses are paid on a linear sliding scale. (Those who score 85 points get the lowest bonus, those who score 100 points get the highest.) |
Previous: Performance Periods
Next: Who Does (and Doesn’t) Take Part in MIPS
DISCLAIMER AND LIMITATION OF LIABILITY: Meeting regulatory requirements is a complicated process involving continually changing rules and the application of judgment to factual situations. The Academy does not guarantee or warrant that regulators and public or private payers will agree with the Academy’s information or recommendations. The Academy shall not be liable to you or any other party to any extent whatsoever for errors in, or omissions from, any such information provided by the Academy, its employees, agents, or representatives.
COPYRIGHT© 2020, American Academy of Ophthalmology, Inc.® All rights reserved. No part of this publication may be reproduced without written permission from the publisher. American Academy of Ophthalmic Executives® and IRIS® Registry, among other marks, are trademarks of the American Academy of Ophthalmology®.
All of the American Academy of Ophthalmology (AAO)–developed quality measures are copyrighted by the AAO’s H. Dunbar Hoskins Jr., MD, Center for Quality Eye Care (see terms of use).