Download PDF
This summer, CMS announced wholesale changes to the quality measure benchmarks in the Merit-Based Incentive Payment System (MIPS).
Why the benchmarks matter. When you report on a quality measure, you can earn achievement points based on how your performance rate compares against a benchmark.
In 2021, these benchmarks are typically based on performance data from 2019, and measures can have different benchmarks depending on whether you report via the IRIS Registry manually; via your electronic health record (EHR) system or IRIS Registry–EHR integration; or via Medicare Part B claims.
Benchmark Deflation!
The quality benchmarks for 2021 were originally published on Dec. 31, 2020.
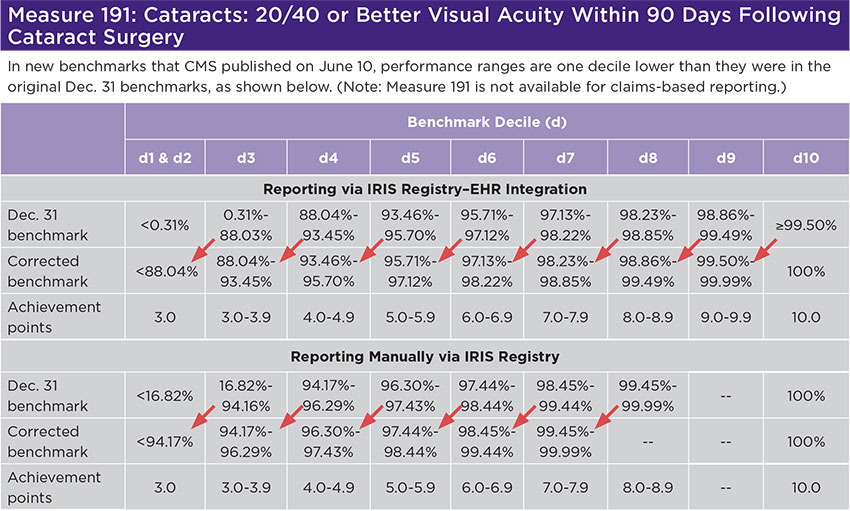
However, CMS made a systematic error that ran through almost all of them: The range of performance rates associated with a particular decile should have been associated with the decile below, as shown in the table for measure 191 (below). Measure 191 has one benchmark for EHR–based reporting and another for reporting manually via the IRIS Registry. For the latter, the benchmark published on Dec. 31 assigned the “99.45%-99.99%” performance range to decile 8, but it should have been assigned to decile 7. Why does this matter? If your performance rate was 99.99%, you would have earned 8.9 achievement points based on the original benchmark—and 7.9 achievement points based on the corrected benchmark. (With a 100% performance rate, you would earn 10 achievement points based on either benchmark.)
CMS published the corrected benchmarks on June 10.
Two Measures Suppressed
On June 30, CMS announced that it was suppressing two measures for those who report via claims:
- Measure 1: Diabetes: Hemoglobin A1c Poor Control (>9%)
- Measure 117: Diabetes: Eye Exam.
Why suppress these two measures? For the 2021 performance year, the specifications of these two measures had been updated: CPT codes were added to the algorithm that is used for determining whether a patient should be included in the numerators for these measures. However, CMS failed to update its systems to reflect these changes. Consequently, the performance rates for these two measures might not be accurate for claims-based reporters. The June 30 announcement only applies to those who are reporting MIPS via claims; it does not impact clinicians who are reporting MIPS via the IRIS Registry.
What does this mean for you? When CMS calculates your quality score, it divides a numerator by a denominator.
The numerator is the sum of your measure achievement points and measure bonus points.
The denominator is based on the total available achievement points, which is typically 60 for ophthalmologists.
If you report measures 1 and/or 117 via claims, they won’t contribute any points to your numerator when CMS calculates your quality score. However, if you reported on one or both of those measures before they were suppressed, CMS has said that it will reduce your denominator by 10 or 20 points, respectively.
Are You Reporting Via Claims?
If you are reporting via Medicare Part B claims, many of the measures available to you are already subject to drastic scoring limitations, such as a 7-point cap on achievement points and scoring that “stalls” at a low decile. Attaining a quality score that is high enough to avoid a MIPS payment penalty was already a tall order; this summer’s benchmark deflation increases the challenge.
Suppression of measure 1 compounds that problem, since it could have been one of the highest-scoring quality measures for ophthalmologists who report via claims, and it also could have earned clinicians 2 high-priority bonus points.
Consider reporting manually via the IRIS Registry. It is not too late to switch to manual reporting via the IRIS Registry (aao.org/iris-registry). There is an Oct. 31 deadline to sign up, but don’t wait until then. You would need to catch up with some additional paperwork (e.g., gathering data-completeness totals) and should get started as soon as possible.
Going Forward
Check that you’re referencing the updated benchmarks. It is important to check that you are using the most current versions of EyeNet’s MIPS 2021: A Primer and Reference (look for “Updated July 2021” on the cover) and IRIS Registry Preparation Kit (at time of press, Version 4). You can download these at aao.org/eyenet/mips-manual-2021 and aao.org/iris-registry/user-guide/getting-started, respectively. You also can purchase a spiral-bound version of the IRIS Registry Preparation Kit at the Academy store.
Watch for future alerts. Check your email for Washington Report Express (Thursdays) and Medicare Physician Payment Update (first Saturday of the month). AAOE members also receive alerts in Practice Management Express (Sundays).
Are you eligible for the hardship exception? If your practice experienced hardship this year due to “extreme and uncontrollable” circumstances—which can include reasons related to COVID-19—you can apply for a hardship exception. CMS is already accepting applications. For more information, visit aao.org/medicare/resources/MIPS-extreme-hardship-exceptions.