By Mike Mott, Contributing Writer, interviewing Ryan Gise, MD, Ashley Khalili, MD, and Ken K. Nischal, MD, FAAP, FRCOphth
Download PDF
MIRM (Mycoplasma pneumoniae-induced rash and mucositis) is an extrapulmonary complication of a respiratory tract infection commonly found in children. Previously identified as atypical Stevens-Johnson syndrome (SJS), it’s now understood by dermatologists to be a distinct—and significantly milder—condition altogether.1
But given some similarities in the ophthalmic manifestations of MIRM and SJS, ophthalmologists should be aware of how MIRM affects the eye, said Ashley Khalili, MD, at Northwell Health in Great Neck, New York. “Because SJS causes significant morbidity and is on the differential, we need to be able to clearly distinguish between the two—for diagnosis, treatment, follow-up, and coordination with the proper specialties.”
What’s Behind MIRM?
M. pneumoniae is a well-known pathogen that causes what’s commonly called “walking pneumonia.” Up to one-quarter of patients with MIRM exhibit mucocutaneous involvement of the eyes, mouth, and urethra, typically sloughing of skin and scarring.2
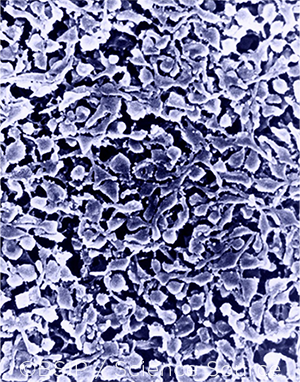
The molecular mechanism behind MIRM has yet to be elucidated, said Ryan Gise, MD, at Boston Children’s Hospital. “This is a theoretically inflammatory disease secondary to Mycoplasma infection that typically occurs in school-age kids, more predominantly in boys,” he said. “But there’s evidence that a MIRM-like illness can be caused by other infections as well, including influenza A and B, adenovirus, Streptococcus, human metapneumovirus, parainfluenza type 2, rhinovirus, and even SARS-CoV-2.”
New nomenclature needed? As a result, said Dr. Gise, some dermatologists are proposing to replace the term MIRM with RIME (reactive infectious mucocutaneous eruption), an umbrella category acknowledging that pathogens other than M. pneumoniae may serve as the trigger for postinfectious rash and mucositis.3,4
 |
|
NOT THE ONLY CAUSE? Although M. pneumoniae (shown here at 10,000× magnification) is the leading culprit, other pathogens may trigger the postinfectious rash and mucositis.
|
MIRM and the Eye
Despite the need for clarity regarding the root cause of MIRM, an increasing number of case studies are shedding light on its ophthalmic manifestations.
Ken K. Nischal, MD, FAAP, FRCOphth, and his team at the University of Pittsburgh Medical Center (UPMC) Children’s Hospital of Pittsburgh were the first to publish a report on MIRM and the eye in 2019.5 In this paper, they described mild ocular involvement: “In the five patients we included, all had inflammatory conjunctivitis, including some adhesions between the tarsal conjunctiva and the bulbar conjunctiva like symblepharon,” said Dr. Nischal. “Two children did have lid margin and conjunctival ulceration, and one experienced recurrent conjunctival pseudomembrane formation, but we didn’t identify any corneal involvement, and the visual outcomes were excellent.”
A more recent chart review by Dr. Gise and his colleagues offers a similar picture.6 “The most common long-term sequelae we found were lid margin scarring or thickening along with blepharitis,” said Dr. Gise. “The vast majority of patients had mild manifestations, a little bit of staining or breakdown of the conjunctiva that was easily managed.” He noted that four of the more severe cases in their 15-patient cohort required an amniotic membrane transplant (AMT) or bilateral placement of a Prokera device (Bio-Tissue) due to worsening corneal involvement. However, none of the patients suffered loss of vision.
In the latest review by Dr. Khalili and a team at Northwell Health, all 10 patients presented with conjunctivitis. Half had pseudomembranes that required daily removal.7 “Corneal involvement was rare,” said Dr. Khalili, “but we did observe notable progression of the disease in half of our MIRM cases, which points to the need for close monitoring and prompt treatment to prevent any potential complications.”
Working Across Specialties
Working in collaboration with dermatology and pediatrics is imperative when treating patients with MIRM, said Dr. Khalili. Your dermatology colleagues not only will coordinate in confirming the diagnosis but also will be essential in managing systemic medications and the often-prominent oral mucositis.
“Urology, gastroenterology, and ENT consultation might also be indicated depending on the location and severity of the mucosal involvement,” she said. “For example, some patients can have severe oral ulcerations that lead to fluid and nutritional deficiencies from decreased oral intake. It’s really important that these patients receive the proper supportive care and pain control.”
|
Diagnosis and Treatment
The differential for patients presenting with MIRM should include SJS, erythema multiforme, and toxic epidermal necrolysis, said Dr. Nischal.
Signs and symptoms. What distinguishes MIRM from these conditions is the prominent involvement of the mucous membranes, said Dr. Khalili. Whereas erythema multiforme typically presents with classic target lesions and SJS with much more extensive skin involvement, MIRM tends to follow a less severe clinical course. In addition, she said, there is a prodrome of cough and fever commonly occurring up to one week prior to mucositis or skin involvement with MIRM. So the keys in diagnosis are the symptoms of the respiratory disease as well as polymerase chain reaction and immunoglobulin M antibody testing.
“But the big question is always, ‘Is this Stevens-Johnson or not?’” said Dr. Nischal. “If it is, then we have to be much more aggressive in terms of treatment because of the much higher risk of permanent ocular surface dysfunction, limbal stem cell insufficiency, ectropion, or symblepharon formation.”
Management. In most cases of MIRM, aggressive intervention is not indicated, as patients tend to improve with medical management alone, said Dr. Khalili. Systemic treatment, which is given in conjunction with dermatology colleagues, typically includes antibiotics and, sometimes, steroids.
Ocular treatment requires aggressive lubrication with both drops and ointments as well as topical anti-inflammatory treatment with steroids and antibiotics if epithelial defects of the conjunctiva or cornea are noted, said Dr. Khalili. Close follow-up is also necessary, she added, especially if pseudomembranes need to be removed. New epithelial defects and staining might also suggest an active process that requires even closer monitoring.
A stepwise approach. At Boston Children’s Hospital, Dr. Gise utilizes a stepwise approach to treat MIRM that is similar to the SJS criteria pioneered by Darren G. Gregory, MD, and his colleagues at the University of Colorado.8
“Even if there is not ocular involvement, we start all of our patients on lubrication and continue to follow closely. Dermatology and our general pediatrics service manage systemic treatment. But the key is ‘the earlier the intervention the better,’ so that we can help decrease disease progression and the need for stronger or more invasive ocular treatments.”
For more moderate disease—for example, staining of less than one-third of the lid margin or conjunctival staining with no corneal involvement—Dr. Gise adds combined antibiotic and steroid eyedrops, typically Tobradex or Maxitrol, along with a steroid ointment. “One drop is always better than two in this population,” he said. “These kids are miserable—and trying to get a drop in them is miserable. So we try to limit that and apply them together.”
Transplant versus Prokera. If the child’s condition progresses further—for example, staining of more than one-third of the lid margin on one or more lids, a corneal epithelial defect, and/or conjunctival staining greater than 1 cm—Dr. Gise would then consider an AMT or a Prokera device after close 24-hour monitoring. “We typically prefer the transplant, because although the Prokera goes into the fornix, it doesn’t go over the lid margin, and that’s the area that’s affected the most.”
For the AMT procedure, Dr. Gise uses a single sheet of amniotic membrane that’s roughly 5 × 10 cm, rather than cutting out and sewing a number of smaller sheets. He places the sheet over the entire mucosal ocular surface, anchoring it with two sutures in the upper eyelid and two in the lower. After tacking down the amniotic membrane and placing it in the fornix, a symblepharon ring keeps everything in place. This procedure takes only about 15 minutes, versus the time needed to sew in multiple sheets, he said.
“Some ophthalmologists might ask why we are so aggressive with an AMT if MIRM is generally so mild,” said Dr. Gise. “But if there are patients who are trending toward severe disease, we feel that we’re minimizing risk [of long-term sequelae] by just putting the transplant in, making the child feel better, and ultimately protecting the corneal surface with a fairly safe and minimally invasive procedure.”
Visual outcomes. Although visual outcomes are significantly better in MIRM than in other disorders on the differential, ophthalmologists should have a low threshold for treatment to avoid permanent sequelae, said Dr. Khalili. “Of the long-term outcomes that have been reported, patients do maintain good vision with no associated comorbidities,” she said. “But dry eye findings have been documented.”
Risk of recurrence. It’s also important to be aware that patients with MIRM are at risk of developing it again, said Dr. Gise. “We’ve seen two patients who had MIRM once and then developed another infection that caused a similar eruption, although [it was] less severe,” he said. As a result, he said, clinicians “should have a high index of suspicion in the future for these kids, because [a similar illness] can be triggered again by what now looks like different types of infections, not just Mycoplasma.”
Anticipating New Research
The distinction between MIRM and SJS was made relatively recently, so ophthalmologists still have a lot to learn about the disease process, said Dr. Nischal. But he expects a jump in MIRM research in the near future that will allow physicians to be more specific in their treatment and improve their ability to forecast prognoses.
___________________________
1 Canavan TN et al. J Am Acad Dermatol. 2015;72(2):239-245.
2 Waites KB, Talkington DF. Clin Microbiol Rev. 2004;17(4):697-728.
3 Mazori DR et al. Pediatr Dermatol. 2020;37(3):545-547.
4 Song A et al. Pediatr Dermatol. 2021;38(5):1222-1225.
5 Shah PR et al. Cornea. 2019;38(10):1305-1308.
6 Gise R et al. Am J Ophthalmol. 2020;219:251-256.
7 Khalili A et al. J AAPOS. 2021;25(6):348.e1-348.e6.
8 Gregory DG. Ophthalmology. 2016;123(8):1653-1658.
___________________________
Dr. Gise is a pediatric ophthalmologist at Boston Children’s Hospital and an instructor of ophthalmology at Harvard Medical School. Relevant financial disclosures: None.
Dr. Khalili is a cornea specialist at Northwell Health in Great Neck, N.Y. Relevant financial disclosures: None.
Dr. Nischal is chief of pediatric ophthalmology, strabismus, and adult motility at the UPMC Children’s Hospital of Pittsburgh and medical director of UPMC Children’s telemedicine program. He also is director of pediatric program development at the UPMC Eye Center and professor of ophthalmology at UPMC in Pittsburgh. Relevant financial disclosures: None.
For full disclosures and the disclosure key, see below.
Full Financial Disclosures
Dr. Gise None.
Dr. Khalili None.
Dr. Nischal Carl Zeiss: C; Essilor Instruments: L; RainBio: C; Santen: C; Vyluma: C.
Disclosure Category
|
Code
|
Description
|
| Consultant/Advisor |
C |
Consultant fee, paid advisory boards, or fees for attending a meeting. |
| Employee |
E |
Employed by a commercial company. |
| Speakers bureau |
L |
Lecture fees or honoraria, travel fees or reimbursements when speaking at the invitation of a commercial company. |
| Equity owner |
O |
Equity ownership/stock options in publicly or privately traded firms, excluding mutual funds. |
| Patents/Royalty |
P |
Patents and/or royalties for intellectual property. |
| Grant support |
S |
Grant support or other financial support to the investigator from all sources, including research support from government agencies (e.g., NIH), foundations, device manufacturers, and/or pharmaceutical companies. |
|