By Diane Donofrio Angelucci, interviewing Viridiana Kocaba, MD, Marcony R. Santhiago, MD, PhD, and William B. Trattler, MD
Download PDF
Clinical studies have shown that corneal cross-linking (CXL) is an effective treatment to strengthen the cornea and reduce progression in patients with keratoconus.1-3 However, in rare cases, intense corneal remodeling occurs after the procedure, according to Marcony R. Santhiago, MD, PhD, who holds appointments in the United States and Brazil. By comparison, the majority of patients have stable readings after the procedure or flattening of up to 1 D or 2 D over 2 years.4
Case reports. Dr. Santhiago described 2 cases of significant corneal flattening and remodeling 1 year after a standard CXL protocol.4
- A 28-year-old woman with progressive bilateral keratoconus was treated in the right eye only. The maximum keratometry (Kmax) in that eye had increased more than 1.0 D during the previous year, and her preoperative steep and flat keratometric readings in the right eye were 59.74 D and 51.94 D, respectively. One year after treatment with standard epithelium-off CXL (3 mW/cm2 for 30 minutes, with a total energy of 5.4 J/cm2), her steep and flat keratometry readings had dropped to 48.80 D and 45.9 D, respectively (a decrease in the differential map of 14 D).
- The second case was a 14-year-old boy with progressive bilateral keratoconus whose right eye was treated. As with the first patient, that eye had demonstrated progression of more than 1.0 D during the previous year. His steep and flat keratometry readings were 63.26 D and 52.91 D, respectively, before he underwent standard epithelium-off CXL. One year later, his steep and flat keratometry readings changed to 56.76 D and 50.40 D, respectively (a decrease in the differential map of approximately 7 D).
Neither patient experienced complications during or immediately after treatment. One year after CXL, both tolerated a gas-permeable contact lens, achieving a corrected distance visual acuity (VA) of 20/25 in the treated eye.
William B. Trattler, MD, of the Center for Excellence in Eye Care in Miami, who has performed CXL continuously over 9 years as part of 2 studies (Peshke, CXLUSA), explained that patients who experience intense corneal reshaping usually have greatly improved vision, as was reported in these 2 cases. “You’re starting off with patients who have advanced keratoconus,” he said. “They have very irregularly shaped corneas. The corneal remodeling resulted in significant reshaping and flattening over the first year following CXL, so the patient’s cornea and vision are moving in the right direction. One expects that with more time, these 2 patients will experience further corneal reshaping.”
Further investigation. Dr. Santhiago continues to study additional cases with intense flattening after standard CXL. Cases such as these raise questions in the refractive surgery community. What physiologic processes are taking place in these eyes? What are the main preoperative factors associated with intense corneal remodeling after CXL? What does this mean for treatment going forward? The conversation is just beginning, with much still to be learned.
Implications
What are the implications of intense flattening?
Physiologic processes. “First, this flattening reveals that there is a potent ongoing remodeling effect in the year after the surgery, and it indicates that there are gradual viscoelastic adjustments in response to the altered distribution of stress imposed by selective stiffening of the cornea relative to the adjacent sclera,” Dr. Santhiago said. “The corneal remodeling, in general, after CXL is probably related, among other things, to intense wound healing, an increase in corneal elasticity, CXL effective depth, and central cone location,” he said.5-7
“This flattening process appears to slowly continue over the years,8 which supports the hypothesis of the long-term effect of CXL,” said Viridiana Kocaba, MD, at the Université Claude Bernard Lyon 1, Edouard Herriot Hospital in Lyon, France.
Dr. Trattler added, “We have patients who have significant corneal reshaping without corneal haze that continues over many years. With continued improvement in corneal shape, patients can typically experience improvement in quality of vision over time.”
Clinical. The clinical ramifications include the following:
Patient selection. A careful preoperative selection of patients is recommended, said Dr. Kocaba. Like other surgical procedures, this decision is based on the balance between benefits and risks, she said, adding that it is important not to underestimate the potential risks and that additional prospective studies are needed to increase selection criteria. Specifically, she pointed out that research such as that by Koller et al. found that preoperative Kmax exceeding 54.0 D was associated with statistically significant corneal flattening during the first year after CXL.9 And Dr. Santhiago said that he’s observed that children’s corneas tend to have more dramatic flattening, but he noted that more data are needed to corroborate this perception.4
Along similar predictive lines, Dr. Santhiago added, “One of our studies is revealing that, although [they are] only mild predictors, the preoperative flat keratometry and the difference between flat and steep keratometry may be some of the indicators of how much that cornea will remodel or flatten.”
Likewise, Dr. Trattler explained that preoperative levels of disease severity can influence the response. “If you have somebody who has mild keratoconus, they will only have a modest amount of corneal flattening,” he said. “If you have someone who has a severe level of keratoconus, they’re more likely to have a more significant response to the treatment.”
Postop care. “These reported cases underline the absolute necessity of a close follow-up of our patients after CXL,” Dr. Kocaba said. After CXL, she usually sees patients at days 1 and 7 and months 1, 3, and 6, depending on the result. If the eye is stable, she sees the patient every 6 months thereafter. Dr. Santhiago added that some studies have shown that the flattening process can continue for 5 years. In fact, Kymionis et al. reported the case of a 23-year-old woman with bilateral CXL who experienced significant flattening and thinning of the cornea in the right eye throughout a 5-year follow-up period while the left eye remained stable.10
Dr. Kocaba noted that excessive corneal flattening after CXL may be associated with deep stromal haze10 or a significant decrease in corneal thickness.11 Dr. Trattler spoke of a patient who experienced inflammation of the cornea in the early postoperative period following epithelium-off CXL. “The patient was treated with topical steroids for the inflammation. However, the patient developed corneal haze and experienced significant corneal flattening,” he said. “While the haze improved over time, the patient still had mild corneal haze along with significant corneal flattening, which resulted in slightly reduced vision compared to the patient’s vision prior to epi-off CXL.”
In light of these potential changes, Dr. Santhiago suggested that any subsequent refractive procedure be delayed until remodeling has occurred. “I believe either contact lens—scleral or not—or intracorneal ring segments [ICRS] are better planned at least 1 year after the surgery.”
A positive? On the flip side, Dr. Santhiago and Dr. Trattler agreed that the intense remodeling has a positive effect in some corneas when there is no need for topography-guided excimer laser procedures or ICRS.
But Dr. Kocaba pointed out, “Even if corneal flattening seems to be a positive side effect, these cases of intense flattening highlight the possible unpredictable response of the cornea after CXL.”
Ongoing Research
Ophthalmologists need to continue investigating the cases in which intense flattening occurs.
Biomechanical data needed. “The indication for CXL is currently based on only one tool—corneal topography,” Dr. Kocaba said. “Changes in corneal topography are still insufficient to provide conclusive evidence of keratoconus progression. That is why corneal biomechanical and biochemical changes might need to be included in this decision. Indeed, understanding biomechanical destabilization of the cornea could probably assist with the management of the keratoconus.”
She added, however, that the processes underlying corneal biomechanical changes after CXL are unclear. Previous studies have shown that while biomechanical properties after ex vivo CXL suggest corneal stiffness, these findings may not be accurate indicators of the in vivo response to CXL.12
“Several in vivo measurements of corneal biomechanics have been developed, such as supersonic shear wave imaging, applanation resonance tonometry, acoustic radiation force, and scanning acoustic microscopy,” she said. These are being studied experimentally.
Confocal microscopy might help. “A progressive reduction in collagen corneal keratocytes has been observed in patients with keratoconus, and the decline in keratocyte density correlates with indices of disease severity,” Dr. Kocaba said.13 In addition, she said, activated keratocytes increase after CXL, possibly indicating greater stromal inflammation.14 She suggested that in vivo confocal microscopy could help identify patients at high risk of intense flattening after CXL.15
Improving Results
As research continues, Dr. Trattler offered recommendations to help ophthalmologists obtain optimum results.
Evaluations. Clinicians need to evaluate key factors in patients with keratoconus, such as uncorrected VA, best-corrected VA, and corneal shape. “You want to be able to compare one visit to the next by looking at comparative topography maps—called difference maps,” he said. At each visit, ophthalmologists can use these difference maps to determine whether keratoconus is stable or whether areas of the cornea are becoming flatter or steeper.
Technique. CXL technique is also important. “Dr. Michael Mrochen has shown that we should center the UV light overlying the thinnest part of the cornea,16 which results in a greater effect,” Dr. Trattler said. “If the thinnest part of the cornea is in the center of the cornea, and a patient is looking directly at the light, then the UV light will be centered over the thinnest part of the cornea and it will travel deeper in the cornea where the cornea is weakest. But if the thinner part of the cornea is significantly inferior to the center, then the UV light rays will hit that part of the cornea at a bit of an angle, resulting in some reflection of light. Therefore, it may help to have the patient look slightly above the UV light, so that the UV light is centered over the thinnest part of the cornea.”
Looking Ahead
While Dr. Santhiago and his colleagues are currently focusing on identifying the main preoperative factors associated with intense corneal remodeling after CXL, he expects that in the future, ophthalmologists will be able to adapt CXL fluence and time according to each patient. “I am positive that we are working toward a more personalized procedure, not only in identifying the individuals who will have the most intense corneal remodeling, but also those who are going to benefit from it,” Dr. Santhiago said.
___________________________
1 Raiskup-Wolf F et al. J Cataract Refract Surg. 2008;34(5):796-801.
2 Caporossi A et al. Am J Ophthalmol. 2010;149(4):585-593.
3 Wittig-Silva C et al. Ophthalmology. 2014;121(4):812-821.
4 Santhiago MR et al. J Refract Surg. 2015;31(6):419-422.
5 Roy AS, Dupps WJ Jr. J Refract Surg. 2009;25(10):875-887.
6 Roy AS, Dupps WJ Jr. Invest Ophthalmol Vis Sci. 2011;52(12):9174-9187.
7 Greenstein SA et al. J Refract Surg. 2012;28(6):397-405.
8 Kymionis GD et al. Cornea. 2014;33(10):1071-1079.
9 Koller T et al. J Cataract Refract Surg. 2011;37(8):1488-1492.
10 Kymionis GD et al. Cornea. 2015;34(6):704-706.
11 Hafezi F et al. Br J Ophthalmol. 2011;95(8):1171-1172.
12 Bekesi N et al. Invest Ophthalmol Vis Sci. 2017;58(3):1612-1620.
13 Bitirgen G et al. Int J Ophthalmol. 2015;8(3):534-539.
14 Aminifard MN et al. Int Ophthalmol. 2015;35(6):785-792.
15 Kocaba V et al. Cornea. 2015;34 (suppl 10):S61-S64.
16 Mrochen MC et al. Poster #D975, Beam profile calculations to increase the volume of cross-linked of corneal tissue. Presented at: ARVO Annual Meeting; May 10, 2012, Fort Lauderdale, Fla.
___________________________
This article has been adapted from a Refractive Surgery Outlook article that was originally published on the International Society of Refractive Society website.
___________________________
Dr. Kocaba is associate professor of ophthalmology at the Université Claude Bernard Lyon 1, Edouard Herriot Hospital in Lyon, France. Relevant financial disclosures: None.
Dr. Santhiago is adjunct professor at the University of Southern California in Los Angeles; professor of ophthalmology at the Federal University of Rio de Janeiro, Brazil; and associate professor of ophthalmology at the University of São Paulo, Brazil. Relevant financial disclosures: None.
Dr. Trattler practices with the Center for Excellence in Eye Care in Miami. Relevant financial disclosures: Avedro: L; CXLO: C,O; CXLUSA: C.
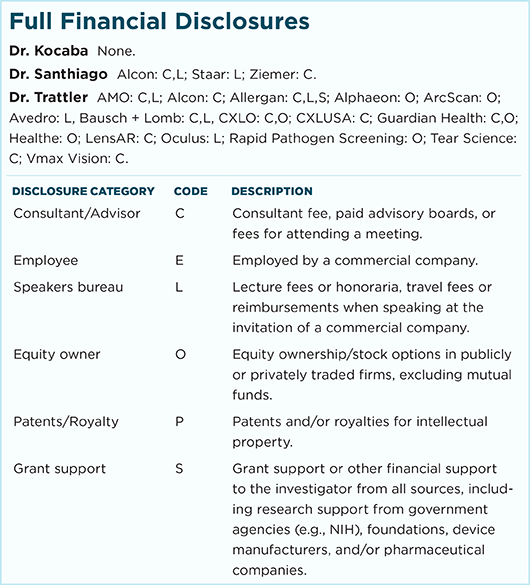
For full disclosures and the disclosure key, see below.