By Laura Huang, BA, Jayanth Sridhar, MD, and Ron L. Lam, MD
Edited by Steven J. Gedde, MD
Download PDF
For three weeks, Rita Jarvis* had been having moderate headaches on a daily basis. The 73-year-old then suddenly developed blurred vision in her left eye and horizontal diplopia. At that point, she saw an ophthalmologist in our community, who diagnosed a sixth cranial nerve palsy, affecting the left side. Her diplopia resolved within a week; unfortunately, this was because she no longer had any vision in her left eye. Ms. Jarvis was then admitted to our hospital and started on intravenous steroids, and we were consulted.
We Get a Look
By the time we evaluated Ms. Jarvis, it was five weeks after her symptoms began, and she was still having mild headaches. She denied having any pain with eye movements, jaw claudication, or scalp tenderness. She also reported no recent or earlier trauma and no sinus congestion or nasal discharge.
Ms. Jarvis’ past medical history was significant for several autoimmune diseases. She had rheumatoid arthritis (which was being treated with hydroxychloroquine, mycophenolate mofetil, and a tapering dose of prednisone), Sjögren syndrome, and hypothyroidism. She also had interstitial lung disease with pulmonary fibrosis, for which she was on home oxygen.
When we examined Ms. Jarvis, her visual acuity was 20/25 in her right eye and no light perception in her left. We noted an afferent pupillary defect, decreased sensation of the ophthalmic nerve, and full motility on forced ductions of the left side. Hertel exophthalmometry showed readings of 24 mm in the right eye and 30 mm in the left. The dilated fundus examination demonstrated extensive bilateral peripapillary atrophy without disc edema or pallor. All other aspects of the exam, including the anterior segment, macula, blood vessels, and intraocular pressures, were within normal limits.
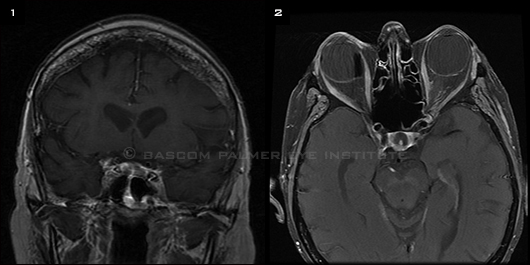
Laboratory results demonstrated an increased white blood cell count of 14.7, with 82 percent polymorphonuclear leukocytes. Initially, the MRI scan of the brain and orbit and results of nasopharyngeal endoscopy were reported as unremarkable, although review of the neuroimaging raised concern for subtle enhancement of the left posterior sphenoid sinus (Fig. 1).
At that time, we determined that Ms. Jarvis suffered from left orbital apex syndrome characterized by optic neuropathy, a sixth nerve palsy, and a partial pupil-sparing third nerve palsy with ophthalmic nerve involvement. We recommended repeating the MRI.
Repeat neuroimaging was performed; it revealed clear worsening enhancement of the left posterior sphenoid sinus involving the left orbital apex (Fig. 2). Ms. Jarvis was taken to the operating room; an infected mass extending into the opticocarotid recess was discovered, excised, and sent for culture and pathology. The primary care team subsequently put her on broad-spectrum antibiotics in addition to the intravenous steroids.
After the surgery, Ms. Jarvis’ relative afferent pupillary defect and ptosis in the left eye remained unchanged, although equal ophthalmic nerve sensation was restored.
|
What's Your Diagnosis?
|
 |
|
(1) The initial T1-weighted MRI coronal scan raised concern for subtle enhancement and thickening along the lateral wall of the left posterior sphenoid sinus. (2) A follow-up T1-weighted axial scan revealed worsening enhancement of the area. Both scans were postgadolinium with fat suppression.
|
Diagnosis
Initial pathology of the sphenoid sinus culture demonstrated septate hyphae interspersed with necrotic sinus tissue. Ms. Jarvis was subsequently put on intravenous amphotericin B based on infectious disease recommendations. Our rheumatology colleagues recommended decreasing the dose of prednisone and discontinuing the mycophenolate mofetil.
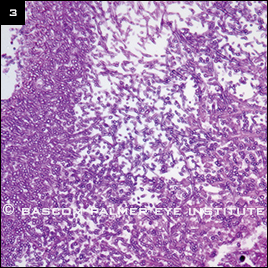
The sinus fungal culture later returned with heavy growth of Aspergillus fumigatus, confirming a diagnosis of sphenoid sinus aspergillosis with invasion of the orbital apex (Fig. 3).
 |
|
CONFIRMATION. Sinus biopsy with HE (hematoxylin and eosin) stain at high magnification shows septate branching hyphae consistent with Aspergillus infection.
|
Our Patient’s Progress
Soon after the diagnosis, Ms. Jarvis began to experience increased difficulty breathing. She was given Bactrim empirically for Pneumocystis jirovecii pneumonia, and her prednisone dose was increased. Review of pathology eliminated the likelihood of mucormycosis, and she discontinued use of amphotericin B to begin oral doses of voriconazole.
One week after admission, Ms. Jarvis decompensated overnight. She was deemed too unstable to undergo a computed tomography angiogram for a clinically suspected pulmonary embolism. She declined intubation or resuscitation and passed away.
Discussion
Sphenoid sinusitis accounts for only 2.7 percent of all nasal sinus infections, with sphenoid sinus aspergillosis representing an even smaller subset.1
Risk factors. Invasive aspergillosis of the paranasal sinuses is a rare and life-threatening disease that occurs most frequently in immunocompromised individuals. Patients who are longtime steroid users or who have neutropenia, hematologic malignancies, aplastic anemia, or diabetes mellitus are most likely to be affected by invasive fungal infections.
Symptoms. The most common symptoms include fever, facial pain, nasal obstruction and discharge, rhinorrhea, epistaxis, and headache. Once infection has spread into the orbit, ophthalmoplegia (involving the third, fourth, and sixth cranial nerves), facial numbness (involving the ophthalmic and maxillary nerves), vision loss (involving the second cranial nerve), ptosis (involving the third cranial nerve and sympathetics), chemosis, proptosis, and pain can result.
Diagnosis. The Aspergillus organism has a characteristic appearance, with narrow, septate hyaline hyphae branched at 45-degree angles that are best seen with Gomori methenamine silver or periodic acid–Schiff staining. Microscopic pathology can show necrosis, vascular invasion, and bony erosion along with septate hyphae. Diagnosis of invasive Aspergillus sinusitis is often delayed, and the condition is commonly mistaken for giant cell arteritis or Tolosa-Hunt syndrome.
In addition, in the paranasal sinuses, aspergillosis and mucormycosis can be almost indistinguishable clinically, with mucormycosis exhibiting broad, nonseptate hyphae with right-angle branching microscopically. Therefore, for best evidence, both a transsphenoidal biopsy from the sinus mucosa and a culture of the organism are recommended. CT and MRI scans may show subtle enhancement of the sinus lining, requiring specific surgical assessment of the sphenoid sinus.
Treatment. Although no definitive and completely effective treatment for invasive Aspergillus exists, management principles include reduction of immunosuppressive medication, surgical debridement, and use of antifungal agents. Treatment of invasive fungal sinusitis with amphotericin B is historically well documented, but it may be complicated by adverse effects.
If both mucormycosis and aspergillosis remain within the differential diagnosis, amphotericin B should be initiated, as Mucor spores are resistant to voriconazole. Once aspergillosis is confirmed, the patient should be switched to voriconazole—or, if the patient is intolerant, to lipid formulations of amphotericin B, which are less toxic. Voriconazole is currently the drug of choice for invasive aspergillosis and is available in both intravenous and oral formulations.2 Duration of treatment should be tailored to the patient’s clinical status, although use of antifungals past any remaining signs of disease is recommended, especially in immunocompromised patients.3
Prognosis. Mortality rates are high, and prognosis may be complicated by mycotic aneurysm, cavernous sinus thrombosis, and intracranial spread.
Reconsidering Our Case
Although there have been cases of invasive aspergillosis affecting the sphenoid sinus, our case of this rare phenomenon is unusual due to the subtle nature of our patient’s presentation. Aside from a mild headache, Ms. Jarvis’ primary symptoms were those of orbital apex syndrome; she did not present with any of the other symptoms that are commonly seen in cases of sphenoid sinusitis. In addition, no abnormalities were evident on either the initial MRI scan or the nasopharyngeal endoscopic exam, highlighting the complex nature of this case.
Summary
Invasive fungal sinusitis carries an extremely high mortality rate and requires early diagnosis and treatment to improve outcomes. This disease should always be considered in the differential diagnosis of orbital apex syndrome, especially in immunocompromised patients. Diagnosis requires early recognition of pathology through biopsy and culture. Treatment involves reducing immunosuppressive drugs, instituting appropriate antifungals, and surgically debriding the infected area.
___________________________
* Patient’s name is fictitious.
___________________________
1 Lee TA et al. Ann Otol Rhinol Laryngol. 2009;118(3):211-217.
2 Walsh TJ et al. Clin Infect Dis. 2008;46(3):327-360.
3 Sivak-Callcott JA et al. Br J Ophthalmol. 2004;88(5):681-687.
Ms. Huang is a medical student at the University of Miami. Dr. Sridhar is a resident in ophthalmology, and Dr. Lam is professor of ophthalmology; both are at the Bascom Palmer Eye Institute. The authors report no related financial interests.
Calling All Cases!
Submit your mysterious case:
Morning Rounds EyeNet Magazine655 Beach Street San Francisco, CA 94109 Phone: 866-561-8558 or 415-561-8500 eyenet@aao.org |