By Sohrab Tofigh, MD, and Rahul T. Pandit, MD
Edited by Steven J. Gedde, MD
Download PDF
It all started with a simple eye scratch. About 14 days before Dave Smith* came to our emergency room, he noted a minor foreign-body sensation in his left eye. The 40-year-old was working outside, but he took the time to go inside and wash his eye out with tap water at the kitchen sink. Unfortunately, that did not solve the problem. Instead, his eye became red and painful, and he developed a severe discharge and significant degree of vision loss in that eye.
Mr. Smith was seen two days after his symptoms began by an optometrist, who prescribed topical ganciclovir gel, prednisolone, and oral valaciclovir. His symptoms worsened, so he visited an ophthalmologist a few days later, who diagnosed a corneal ulcer and obtained corneal scrapings for staining and cultures. The ophthalmologist discontinued Mr. Smith’s prior therapy and prescribed fortified topical vancomycin and ceftazidime drops to be applied every hour.
Two days later, the cultures grew mold. The ophthalmologist switched Mr. Smith’s topical regimen to natamycin 5 percent every hour, moxifloxacin 0.5 percent every two hours, 50 mg/cc of ceftazidime every six hours, and atropine 1 percent twice a day. Mr. Smith’s eye was painful and he could not use his drops consistently; as a result, he came to our ER for further evaluation.
We Get a Look
When we saw Mr. Smith, he was in intense pain and was notably anxious. We could easily note the copious white-yellow thick discharge from his left eye. He mentioned to us that he had not been consistently applying the topical drops due to lack of sleep and increasing anxiety about his worsening vision.
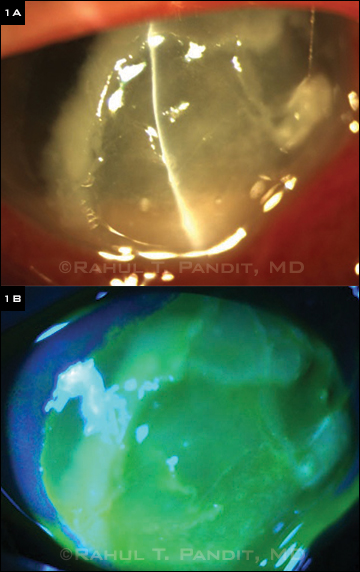
Our examination revealed normal best-corrected visual acuity (BCVA) in his right eye; the BCVA in his left eye was now hand motion. He had severe eyelid swelling and erythema with secondary ptosis in the left eye. The conjunctiva in that eye was diffusely injected, and our examination revealed a large ulcer involving almost the entire cornea, leaving only a small perilimbal rim unaffected in the superior and nasal quadrants. The infiltrate was densest inferiorly, and there appeared to be up to 50 percent thinning of the cornea. The left anterior chamber, iris, lens, and fundus could not be fully assessed because of the density of the corneal ulcer (Fig. 1A and 1B).
|
What's Your Diagnosis?
|
 |
|
(1A) The corneal ulcer’s density made it difficult to assess the anterior chamber, iris, lens, and fundus. (1B) Fluorescein staining revealed the extent of the defect.
|
Critical Decisions
We decided to admit Mr. Smith to the hospital. We based our decision not only on the severity of the corneal ulcer but also on his lack of social support, precarious emotional state, and inability to administer the needed topical medications every hour.
We obtained Mr. Smith’s medical records and laboratory results from his community-based physicians and discussed his case with his primary ophthalmologist. Over the following two days, he was followed closely by our cornea service. Fortunately, he began to show several signs of clinical improvement, including decreasing size of the infiltrate and epithelial defect.
Perhaps more important, his psychological state improved dramatically with the sleep and direct care he received in the hospital. His updated cornea culture revealed the presence of Fusarium fungal species; as a result, his medical management was changed to topical natamycin and moxifloxacin every hour. He was then discharged home with instructions to follow up as an outpatient.
The Second Challenge
On Mr. Smith’s frequent follow-up visits, we noted that the corneal ulcer, after initially improving, had begun to worsen again, even though he said he was applying his medications as prescribed. We changed his regimen to oral voriconazole 200 mg twice daily and topical voriconazole 1 percent every hour.
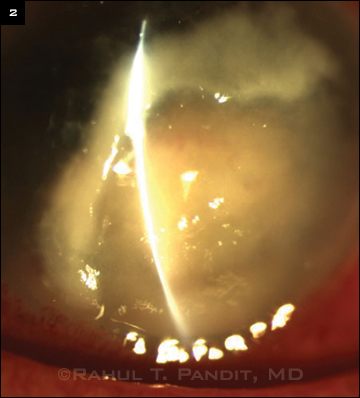
Although his symptoms initially improved (Fig. 2), within two to three days his corneal inflammation began to increase again, and an anterior chamber inflammatory mass was noted. Given the concern for intraocular invasion, we decided to immediately proceed with penetrating keratoplasty (PK).
At the beginning of surgery, a sterile anterior chamber tap was performed to examine the aqueous for fungal elements. The remainder of the surgery included a large PK graft (9-mm donor into 8.5-mm host), removal of the anterior chamber mass, synechiolysis, and removal of a pupillary membrane. At the end of the operation, Mr. Smith received an intracameral injection of amphotericin B and subconjunctival injections of amphotericin B, dexamethasone, and vancomycin. He was then placed on oral and topical voriconazole, as well as topical cyclopentolate 1 percent and moxifloxacin.
We withheld topical steroid therapy at this point, but we placed Mr. Smith on cyclosporine for its anti-inflammatory and antifungal properties.1 Two weeks after surgery, given the lack of any recurrent corneal infiltrate, topical steroids were initiated at a low dose and then increased to combat any likelihood of early graft rejection.
One month after surgery, Mr. Smith was tapered off his antifungal therapy. By two months after surgery, the BCVA in his left eye had improved from hand motion to 20/200.
 |
|
INITIAL IMPROVEMENT. After the patient was discharged from the hospital, the corneal infiltrate improved slightly.
|
Discussion
Our challenges with this clinical case were numerous, from managing a patient who initially had significant problems with compliance to changing and adjusting our medical management once the gold-standard treatment failed to improve the outcome.
Physical and psychological management. Corneal ulcers, especially ones with fungal etiology, are known to be painful and difficult to manage. The first line of treatment for these infections involves application of topical medications every one to two hours. This, along with the significant pain and anxiety that is inherent with such a diagnosis, contributed to our patient’s noncompliance.
In addition, Mr. Smith lacked an adequate social support system. As social support can play a major role in improving compliance with treatment,2 ophthalmologists must not only treat the eye disease but also manage possible aspects of noncompliance. Once the likelihood of high noncompliance rate is confirmed, it is appropriate to admit the patient to the hospital or to arrange for home health care. These options increase the odds of continuous care and application of medications and thus could ultimately save the patient’s vision.
Tailoring treatment. Based on the results of the Mycotic Ulcer Treatment Trial (MUTT), we expected that the outcome of treating Mr. Smith’s filamentous corneal ulcer with topical natamycin would be superior to that of topical voriconazole.3
Nonetheless, our patient did not seem to respond to the natamycin for very long, and he actually seemed to do better on voriconazole. It should be noted, however, that one of the inclusion criteria for the MUTT was an initial visual acuity within the range of 20/40 and 20/400, whereas Mr. Smith’s initial presenting BCVA was far worse at hand motion.
Conclusion
Management of such complex infections is always unique to the individual patient. This case demonstrates the importance of integrating clinical experience and any unique patient characteristics with the most recent and reliable scientific data. It also illustrates the impact of psychological health and social support on the overall success of treating complex and debilitating diseases. Finally, our case serves as a reminder that recommended management always requires adjustments and alterations.
___________________________
* Patient’s name is fictitious.
___________________________
1 Pandit RT. Cornea. 2003;22(1):92-93.
2 Jin J et al. Ther Clin Risk Manag. 2008;4(1):269-286.
3 Prajna NV et al. JAMA Ophthalmol. 2013;131(4):422-429.
___________________________
Dr. Tofigh is a third-year ophthalmology resident at the University of Texas Medical Branch in Galveston, and Dr. Pandit is assistant professor of ophthalmology at Weill Cornell Medical College at Houston Methodist Hospital. The authors report no related financial interests.