By Andrew Stacey, MD, Erin L. McKean, MD, and Jonathan D. Trobe, MD
Edited by Steven J. Gedde, MD
Download PDF
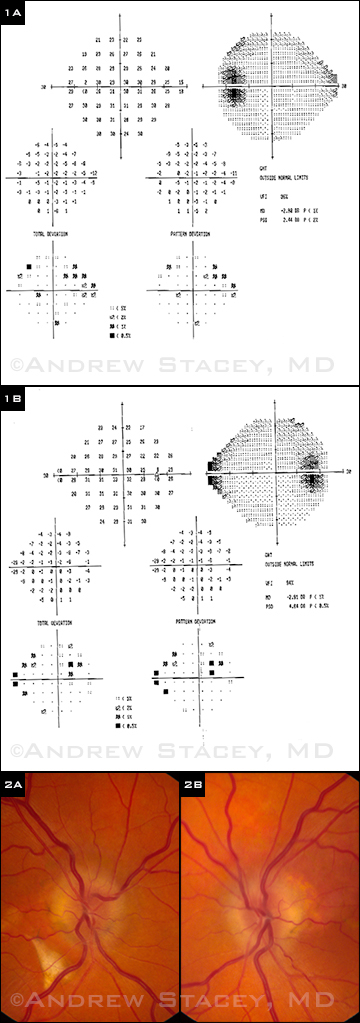
Pete Nye,* a 64-year-old minister, began to notice brief episodes of double vision. He had been diagnosed with a small macular hole in his left eye 25 years earlier but had no other significant ocular history. He consulted an ophthalmologist, who found optic disc elevation in both eyes and abnormal visual fields (Fig. 1). A lumbar puncture revealed an opening pressure of 39 cm water; the cerebrospinal fluid (CSF) was normal. He was diagnosed with idiopathic intracranial hypertension (IIH), prescribed 1 gram of acetazolamide daily, and referred to our office.
A Change of Medications
By the time we saw Mr. Nye, he had decided that he could not tolerate the acetazolamide because it slowed his reaction time and thinking. He did not trust himself behind the wheel of his car—and while officiating at a marriage, he became confused about which notes and scriptures to read.
When we examined him, his best-corrected visual acuity was 20/20 in his right eye and 20/40 in his left. He had normal color vision, Amsler grid test results, and ocular motility. His Humphrey visual fields were unchanged from the previous exam. We noted the presence of bilateral optic disc edema (Fig. 2) and confirmed the diagnosis of IIH. We discontinued the acetazolamide and substituted 40 mg/ day of furosemide.
|
What's Your Diagnosis?
|
 |
|
At presentation, the patient’s visual fields (1A, 1B) were abnormal, and he had bilateral optic disc edema (2A, 2B).
|
The Plot Thickens; the Dura Thins
For the next six months, frequent eye examinations disclosed no change in Mr. Nye’s status. However, one day while he was at the barber shop, a gush of clear fluid drained from his nose when he leaned forward to allow the barber to cut his neck hair. He attributed the watery discharge to a common cold.
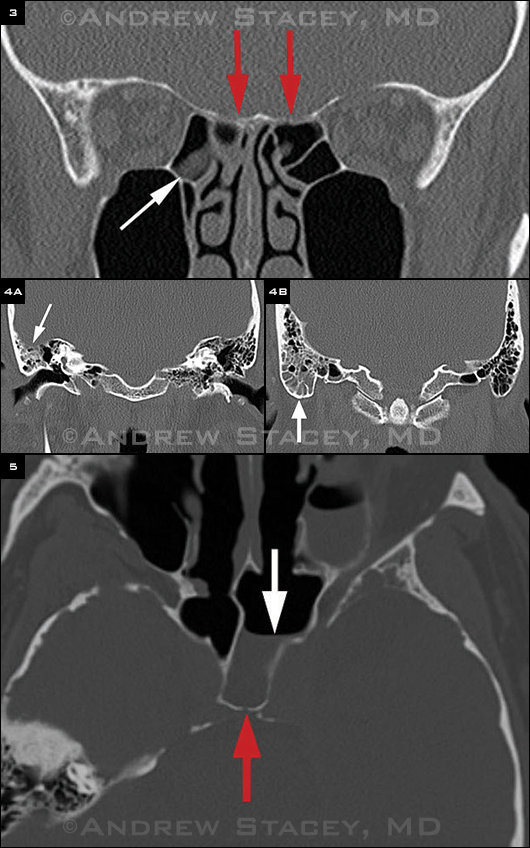
Over the next day, however, his nasal discharge increased in volume. Mr. Nye came to our emergency room, where he underwent a computed tomography (CT) scan of the head (Fig. 3). On the basis of the fluid in the right ethmoid sinuses and thin olfactory grooves, he received a presumptive diagnosis of a spontaneous cribriform plate CSF leak. He underwent bilateral endoscopic skull base repair with free mucosal grafts.
More Trouble
Mr. Nye was asymptomatic until two months after the surgery, when he reported high-pitched tinnitus as well as a feeling of fullness around his right ear, which seemed to be worse in the supine position.
At this time, a physical exam revealed an intact right tympanic membrane with a clear air-fluid level in the right middle ear. A CT scan demonstrated a middle cranial fossa bony dehiscence with fluid in the right mastoid cavity (Fig. 4). Mr. Nye returned to the operating room, where the right middle cranial fossa floor was found to have numerous defects and encephaloceles extending into the middle ear and air cell system. The leak was repaired with split calvarial bone graft and synthetic bone cement to the middle fossa floor via a transtemporal approach.
 |
|
ADDITIONAL EVIDENCE. (3) A coronal CT scan six months after presentation shows fluid in the right ethmoid sinuses (white arrow); both olfactory grooves are thin (red arrows). The suspected diagnosis was cribriform CSF leak. COMPLICATIONS. Coronal CT scan two months after cribriform plate surgery for CSF leak, showing middle fossa bony dehiscence (4A) and fluid in right mastoid cavity (4B). These radiographic signs point to a middle cranial fossa CSF leak. (5) CT scan one year after temporal bone repair of the CSF leak shows fluid in the left sphenoid sinus (white arrow), and a subtle sphenoid bony dehiscence (red arrow) not evident on previous scans. These findings suggested a CSF leak in the sphenoid sinus.
|
More Problems, Then Success
Mr. Nye had no further complaints for another year, when he presented again to our ER with recurrent rhinorrhea and severe headache and neck stiffness. Fluid from his nose tested positive for beta-2 transferrin, confirming that he was suffering a third CSF leak.
The ophthalmologic exam was normal. CSF obtained by lumbar puncture showed signs of bacterial meningitis; cultures grew pneumococcal organisms. A CT scan showed fluid in the left sphenoid sinus and a subtle sphenoid bony dehiscence (Fig. 5). These findings suggested a CSF leak into the sphenoid sinus.
Mr. Nye was treated with intravenous antibiotics that rapidly resolved his headache and neck stiffness. The sphenoid sinus leak was repaired, and he underwent ventriculo-peritoneal shunting. Six months later, he was free of symptoms and his eye examination was normal (Fig. 6).
 |
|
RESOLUTION. Six months after the third repaired CSF leak and placement of a ventriculo-peritoneal shunt, the optic discs are no longer swollen.
|
Discussion
Although it is a rare occurrence, IIH may cause spontaneous CSF leakage, because the high intracranial pressure erodes dura, which may have preexisting weak points.
There have been more than 20 reported cases of primary spontaneous CSF leaks occurring secondary to IIH.1,2 To our knowledge, however, CSF leak in IIH has not been reported to give rise to meningitis.
Noncontrast, high-resolution CT scanning (1.25 mm or finer) is now the most commonly used modality for identification of skull base dehiscences in the setting of CSF rhinorrhea. With CT or radionuclide cisternography, false negatives may occur unless there is an ongoing leak. Furthermore, these studies are invasive and add little to good clinical acumen, high-resolution CT scanning, and endoscopic evaluation. Even so, in rare circumstances, cisternography may be helpful.
At our institution, we will perform an intrathecal fluorescein injection intraoperatively to assist in visualization of the defect in the following settings: 1) If there is not a clear site of skull base dehiscence on high-resolution imaging, 2) if we suspect multiple leak sites, 3) or, in rare circumstances, if we are repairing recurrent leaks in order to assess the quality of the repair.
The standard treatment for CSF leak is direct closure of the hole. But if that is not successful, or if the patient has had meningitis, one must also relieve intracranial pressure by CSF shunt.
Conclusion
The possibility of a CSF leak is often overlooked. Ophthalmologists who manage IIH should ask patients if they have a very runny nose—if the fluid is watery, it could be CSF. A fine-section maxillofacial CT scan usually discloses the presumptive hole. Sealing the hole may not definitively solve the problem, as leakage may occur again in the same place or elsewhere. In IIH, relieving the intracranial pressure by CSF shunt will often be necessary, as in this case. Prompt recognition of a CSF leak in IIH may be life-saving.
___________________________
*Patient’s name is fictitious.
___________________________
1 Yang Z et al. J Neurosurg. 2011;115(1):165-170.
2 Rosenfeld E et al. J Neuroophthalmol. 2013;251(7):1771-1775.
___________________________
Dr. Stacey is a resident in ophthalmology, Dr. McKean is assistant professor of otolaryngology, and Dr. Trobe is professor of ophthalmology and visual sciences and professor of neurology; all are at the University of Michigan in Ann Arbor. The authors report no related financial interests.
___________________________
NEXT MONTH. Read about the case of a curious scratch.