By Surbhi Bansal, MD, and Sandra L. Everett, MD
Edited by Steven J. Gedde, MD
Download PDF
Anthony Roberts* is a 35-year-old bridge painter who wore daily disposable contact lenses. His problems started at work one day, as the work crew was getting ready to go home. After taking off his protective hood, he experienced a foreign body sensation bilaterally. He removed his contact lenses and used water from the onsite wash station to flush his eyes. Because of continuing irritation, he went to a local emergency room, where he was diagnosed with a corneal abrasion in his right eye. He was referred to a local ophthalmologist who treated the corneal abrasion with gatifloxacin and loteprednol etabonate. The exam of the left eye was normal. The abrasion healed, but four weeks later he developed an apparently spontaneous infectious keratitis in his left eye and was referred to our clinic.
We Get a Look
When we saw Mr. Roberts, his Snellen visual acuity was 20/40 in the right eye and counting fingers in the left. In the right eye, we noted a paracentral superotemporal corneal opacity in the area of the previous abrasion. In the left eye, there was a large central epithelial defect, measuring 4.2 mm × 4.4 mm, with a surrounding infiltrate, as well as active iritis. Bacterial, fungal, protozoal (Acanthamoeba), and viral stains and cultures of the left eye were obtained. We suspected that the water from the wash station, which later was reported to have come from a nearby creek, was contaminated.
We start treatment. Pending the results of the cultures, we initiated fortified vancomycin (25 mg/mL), ciprofloxacin, atropine, natamycin, a biguanide, and oral valacyclovir. After the defect in the left eye healed, we prescribed steroids.
Eight weeks after the injury, visual acuity remained 20/40 in the right eye and improved to 20/25 in the left eye as the infection resolved. All stains and cultures were negative. Steroids were tapered off, and all other medications were discontinued.
Problems return. One week later (nine weeks after the initial injury), the patient complained of halos and increased photophobia in the right eye. An additional paracentral opacity below the visual axis was noted in the right eye without anterior chamber reaction. We suspected that an underlying viral infection had reactivated. Antivirals were restarted, and, for several weeks, Mr. Roberts’ visual course fluctuated.
Five weeks after the antivirals were restarted (14 weeks after the initial injury), the visual course deteriorated, with an enlarging epithelial defect and a hypopyon in the right eye. The intraocular pressure in the right eye rose to 45 mmHg, which we attributed to uveitic glaucoma. We restarted fortified antibiotics for the epithelial defect in addition to the antivirals and glaucoma drops that he was already taking. Bacterial and fungal cultures, as well as viral polymerase chain reaction (PCR), were repeated. The possibility of atypical mycobacterial keratitis was also considered.
The first two cultures were negative, but Actinobacillus (formerly Pasteurella ureae), a gram-negative organism, was revealed by a third culture. In this deep-needle corneal culture, a 6-0 silk on G-6 needle (reverse cutting) was passed through the area of the suspected infection nidus in the cornea at 80 to 90 percent depth for the entire length of the suture, and then pieces of this suture were cut and placed on standard culture plates while the needle-end with a small tail of the suture was placed in thioglycollate broth. It was now 16 weeks since the initial injury had occurred.
We try broad-spectrum coverage with antibiotics, antivirals, and antifungals. Despite tailored antibiotic therapy for this gram-negative organism, the right cornea deteriorated further and developed a corneal ulcer. Given the refractory nature of the infection, medical therapy was broadened to cover gram-negative and gram-positive bacteria, as well as viral, fungal, and Acanthamoeba organisms. But the right eye became unresponsive to all antibiotic and antiviral treatment and developed a perforated corneal ulcer for which a penetrating keratoplasty was performed.
The graft failed and the right eye became phthisical. The right eye was enucleated, and Mr. Roberts was fitted with a prosthesis. The left eye developed a visually significant corneal scar.
|
What's Your Diagnosis?
|
 |
|
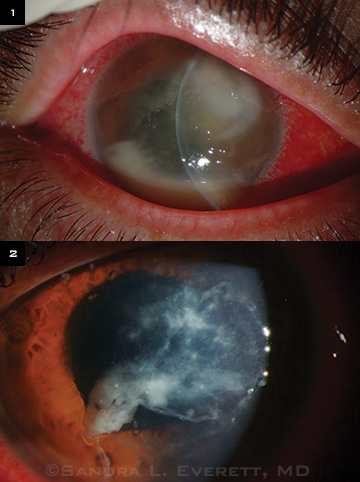
(1) In the right eye, in the areas of the initial corneal abrasion, there was a sudden onset of enlarging corneal epithelial defects with infiltrate 14 weeks postinjury. (2) In the left eye, keratitis at four weeks postinjury resolved slowly, leaving a significant stromal scar.
|
What Final Tests Revealed
The corneal button from the penetrating keratoplasty of the right eye was sent to the New York State Department of Health for further identification by means of 16s rRNA analysis. This revealed growth of endospore-forming gram-positive Bacillus megaterium.
Discussion
Incidence. Bacillus bacterial species account for 1.4 to 2 percent of all bacterial keratitis. They have been associated with endogenous endophthalmitis, posttraumatic or postsurgical keratitis, and contact lens–associated keratitis.1 Although Bacillus infections are aggressive, usually leading to blindness and enucleation, complete recovery has been reported.2
Characteristics. Genus Bacillus contains more than 50 species of aerobic or facultatively anaerobic gram-positive or gram-variable spore-forming rod bacteria. Spore formation can enhance survival in variable temperatures (3 to 75 degrees Celsius) and acidity (pH 2 to pH 10).3,4 Spores are reported to be 100,000 times more resistant to heat and seven to 50 times more resistant to ultraviolet irradiation than vegetatively growing cells.
B. megaterium is a gram-positive, rod-shaped, mainly aerobic spore-forming bacterium. It is found in widely diverse habitats, including soil, seawater, sediment, rice paddies, honey, fish, and dried food. B. megaterium has been reported to sporulate within 36 hours and can survive in various temperatures for up to five months.4
Staining. Gram-positive staining of B. megaterium can be variable, and in Mr. Roberts’ case, this probably led to an initial incorrect laboratory diagnosis of gram-negative A. ureae. When the bacteria are in active infectious phase, cultures can be obtained on blood agar and MacConkey agar plates. The endospore phase can be stained with special stains such as Moeller and Schaeffer-Fulton. Once this microbe is identified, treatment with antibiotics covering gram-positive organisms during the active infectious phase is recommended.
Contact lenses. Although our patient was a daily disposable contact lens wearer, we believe his bilateral infections were more likely to have been caused by exposure to contaminated water than by contact lens use. Gram-negative bacteria are known to be associated with soft contact lens wear with an increased incidence (15- to 20-fold) of ulcerative keratitis.5 However, in this case, the identified organism was gram positive, and gram-positive bacteria are much less frequently reported in contact lens–associated keratitis. B. megaterium has not been cited in the literature as a cause of contact lens keratitis and has not been implicated in FDA recalls of contact lens solutions. It is important to note that the paucity of literature about the role of this organism in eye infections may be due to the difficulty of its isolation and identification in the laboratory.
Initial delayed progression. The prolonged endospore phase of B. megaterium may explain the apparently quiet corneal state in the right eye, while the early vegetative growth phase resulted in the active inflammation in the left eye, at the time we first examined the patient. The delayed progression is also attributable in part to the manner in which this bacterium destroys tissue; it is not only the mere presence of many bacterial cells but also the production of toxins by the cells that causes cellular and tissue damage. This is well documented for the Bacillus species.
In Mr. Roberts’ case, the eventual rapid and aggressive course of B. megaterium and the misleading identification of a gram-negative organism in one of the cultures, which led to incorrect tailoring of antibiotic therapy, contributed to perforation and loss of the right eye.
Summary. Bacillus species should be part of the differential diagnoses of refractory keratitis cases in a suitable context such as exposure to or contamination with soil, seawater, sediment, water from rice paddies, honey, fish, and dried food. Early deep-needle corneal suture cultures may be tried, and special ribosomal nucleic acid tests such as 16s rRNA analysis can be obtained in cases of conflicting lab reports with initial microbial cultures.
___________________________
* Patient name is fictitious.
___________________________
1 Pinna A et al. Ophthalmology. 2001;108(10):1830-1834.
2 Das T et al. Ophthalmology. 2001;108(10):1819-1825.
3 Vary PS et al. Appl Microbiol Biotechnol. 2007;76(5):957-967.
4 Gomathy M et al. Indian J Microbiol. 2007;47(3):259-262.
5 Matthews T et al. Arch Ophthalmol. 1992;110(11):1559-1562.
___________________________
Dr. Bansal is a glaucoma fellow at University of Michigan, Ann Arbor. Dr. Everett is a clinical associate professor of ophthalmology at State University of New York at Buffalo. The authors report no related financial interests.