By Rachelle A. Rebong, MD, Sara J. Haug, MD, PhD, Alan Lowinger, MD, and Emmett T. Cunningham Jr., MD, PhD, MPH
Edited by Steven J. Gedde, MD
Download PDF
Henry Shin* had a terrible headache. The 47-year-old Chinese American furniture mover was usually able to work through aches and pains, but this headache had continued for the past two weeks. He tried over-the-counter medicines—and acupuncture—but nothing seemed to help. When he noticed his vision becoming more blurry, he decided it was finally time to see a doctor.
We Get a Look
By the time Mr. Shin reached our clinic, he had already seen his primary care doctor and general ophthalmologist, who diagnosed him with possible central serous chorioretinopathy. When we saw Mr. Shin, he complained of blurry vision, photophobia, left-sided pulsating headaches, and, on further questioning, left-sided tinnitus. His past ocular history was notable for penetrating trauma from a ski pole injury to the left eye when he was 12 years old. He underwent surgical repair at the time and was able to regain some vision. Past medical, surgical, social, and family histories were otherwise unremarkable.
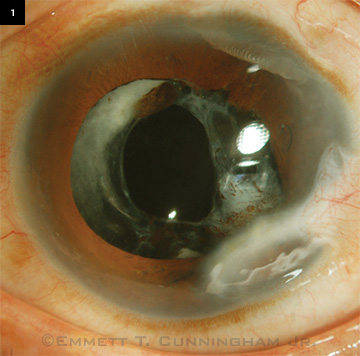
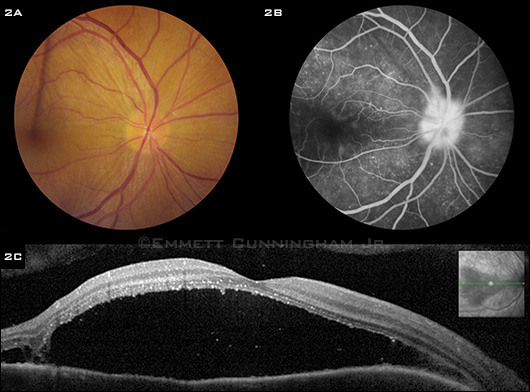
On examination, BCVA was 20/100 in the right eye and counting fingers at 6 feet in the left eye. There was no afferent pupillary defect, and his intraocular pressure was normal in both eyes. Anterior segment examination of the right eye revealed moderate anterior chamber cells, while the left showed several peripheral corneal scars with areas of iridocorneal touch, large, pigmented keratic precipitates on the inferior corneal endothelium, iris atrophy, moderate anterior chamber cells, and aphakia (Fig. 1). Posterior segment examination revealed mild vitreous inflammation, mild hyperemia of the disc, and serous macular detachment in both eyes (Fig. 2A). Fluorescein angiography (FA) revealed late pinpoint hyperfluorescence at the level of the retinal pigment epithelium (RPE) with late, progressive filling of the serous retinal detachment spaces and late leakage of the optic discs bilaterally (Fig. 2B). Spectral domain ocular coherence tomography (SD-OCT) confirmed the presence of bilateral serous macular detachments (Fig. 2C).
|
What's Your Diagnosis
|
 |
|
WE GET A LOOK. At presentation to us, his BCVA was 20/100 on the right and counting fingers at 6 feet on the left. Both eyes had moderately severe panuveitis. Peripheral corneal scars are evident in the left eye, now aphakic, following a penetrating injury 35 years prior to presentation.
|
Workup and Treatment
A laboratory workup was obtained, including the following tests: serum rapid plasma reagin (RPR), fluorescent treponemal antibody absorption (FTAABS), angiotensin-converting enzyme ACE, lysozyme, QuantiFERON-TB (for tuberculosis), complete blood count (CBC), and liver function tests (LFT). All results were either negative or within normal limits. A chest x-ray was also ordered and was normal. Although Vogt-Koyanagi-Harada (VKH) disease can have a presentation very similar to this patient’s condition, his history of penetrating eye trauma together with his clinical findings of bilateral panuveitis with serous macular detachment led to the diagnosis of sympathetic ophthalmia (SO).
While waiting for the final results of his laboratory examinations, we started Mr. Shin on 100 mg of oral prednisone daily, as well as topical prednisolone acetate and homatropine eye drops. After his studies came back as negative or within normal limits, we added oral azathioprine at a dosage of 50 mg daily. Over the course of several months, as the inflammation and subretinal fluid resolved, we were able to taper Mr. Shin off the oral prednisone and topical medications. Meanwhile, the azathioprine was increased to a dosage of 200 mg daily, with close monitoring of his CBC and LFT. Visual acuity at his last visit, 17 months after his initial presentation, was 20/25 in the right eye and 20/400 in the left eye.
 |
|
RIGHT EYE. (2A) Color photograph, (2B) late-phase FA, and (2C) SD-OCT at presentation to us showing optic disc hyperemia, a serous macular detachment, and pinpoint late leakage at the level of the RPE with slow, progressive filling of the serous macular detachment space. We noted similar findings in the left eye.
|
Discussion
Sympathetic ophthalmia is a rare bilateral granulomatous uveitis that occurs following eye trauma or surgery. The eye that experienced the trauma or surgery is referred to as the exciting or inciting eye, whereas the fellow eye is called the sympathizing eye. Inciting events can include any type of injury or surgery—from an ocular contusion to a ruptured globe, and from penetrating procedures such as cataract surgery or vitrectomy to nonpenetrating procedures such as cyclocryotherapy and proton beam irradiation.
How long until onset? The time from ocular injury to onset of SO can vary widely, from two weeks to over 50 years, but approximately 80 percent of cases occur within three months and 90 percent occur within one year.1 Past studies estimated the incidence of SO to be 0.1 percent following intraocular surgery and 0.2 to 0.5 percent after open globe injury. A more recent study looked at the incidence of SO in 59 million citizens of the United Kingdom and Ireland over a 15-month period. It found an incidence of 0.03 per 100,000 population, with the most common risk factor being ocular surgery, especially retinal surgery.2
How does it develop? The cause of SO is unclear. Current theories point to an autoimmune response directed against one or more uveal antigens following trauma or surgery. Genetic factors may also play a role, since associations with major histocompatibility complex (MHC) haplotypes HLADR4/DQw3, HLA-DR4/DRw52, HLAA11, HLA-B40, HLA-DRB1*04, and HLA-DQB1*04 have been shown.1
How is it diagnosed? The diagnosis of SO is based primarily on a consistent clinical history and findings. Laboratory studies are used to rule out other diagnoses, including sarcoidosis, tuberculosis, and syphilis. B-scan ultrasonography is used to exclude posterior scleritis.1
SO should be considered in all patients with bilateral uveitis and history of ocular trauma or surgery. Typical symptoms include blurry vision, pain, and photophobia. Anterior segment examination may show conjunctival injection, anterior chamber inflammation, large or small keratic precipitates, and posterior synechiae. Posterior segment examination may show moderate to severe vitritis, papillitis, exudative retinal detachments, and yellow-white choroidal lesions known as Dalen-Fuchs nodules. Extraocular findings are uncommon but can include headache, hearing disturbance, alopecia, poliosis, and vitiligo, as seen in VKH disease. Ocular complications can include secondary glaucoma, cataract, macular scarring or atrophy, optic atrophy, and, rarely, choroidal neovascularization. Phthisis of the sympathizing eye can occur, but it is uncommon with prompt and aggressive use of immunosuppressive agents.3
What do you look for in imaging? FA often shows punctate hyperfluorescence at the level of the RPE followed by progressive filling of serous detachment spaces, as in our patient. Dalen-Fuchs nodules, which are present in 25 to 30 percent of cases, may be either hypo- or hyperfluorescent, depending on the state of the overlying RPE. Disc leakage and macular edema may occur. SD-OCT can show serous retinal detachments, disorganization and thinning of the retina, and choroidal thickening.4
What does histopathology show? There is a diffuse, bilateral granulomatous nonnecrotizing inflammatory reaction. Thickening of the choroid results from infiltration of mononuclear and epithelioid cells. The choriocapillaris and retina are often, but not always, spared. Dalen-Fuchs nodules appear as collections of lymphocytes, histiocytes, and depigmented RPE cells beneath Bruch’s membrane.3
How is it treated? Systemic corticosteroids constitute the first-line therapy for SO. A usual starting point is high-dose oral prednisone (1-2 mg/kg/day), although severe cases may be started on intravenous pulsed corticosteroids (methylprednisolone 1 g/day for three days) followed by oral prednisone. Topical corticosteroids and cycloplegics are used as adjuncts.
Most patients require long-term treatment with a noncorticosteroid immunosuppressive agent such as azathioprine, methotrexate, or mycophenolate mofetil. Systemic corticosteroids are typically tapered over two to three months, whereas noncorticosteroid immunosuppressive agents tend to be continued for two or more years. More severe cases may require treatment with a DNA crosslinking agent such as chlorambucil or a tumor necrosis factor-alpha (TNF-α) inhibitor such as adalimumab or infliximab.5
Summary. The differential diagnosis for any postoperative or posttraumatic bilateral panuveitis should include SO.6 Most cases occur within three months of the inciting event, although uveitis may appear many years later, as in this case. Medical therapy with systemic corticosteroids and noncorticosteroid immunosuppressive agents is the mainstay of treatment.
___________________________
*Patient name is fictitious.
___________________________
1 Castiblanco CP, Adelman RA. Graefes Arch Clin Exp Ophthalmol. 2009;247(3):289-302.
2 Kilmartin DJ et al. Br J Ophthalmol. 2000;84(3):259-263.
3 Chu XK, Chan CC. J Ophthalmic Inflamm Infect. 2013;3(1):49.
4 Castiblanco C, Adelman RA. Int Ophthalmol Clin. 2012;52(4):173-181.
5 Damico FM et al. Semin Ophthalmol. 2005;20(3):191-197.
6 Doshi RR et al. Am J Ophthalmol. 2010;150(3):295-304.
___________________________
Dr. Rebong is a resident at California Pacific Medical Center (CPMC). Dr. Lowinger is assistant professor of ophthalmology at New England Eye Center and Tufts University School of Medicine. Dr. Haug is in private practice at West Coast Retina Medical Group. Dr. Cunningham is director of the uveitis service at CMPC, adjunct clinical professor of ophthalmology at Stanford University School of Medicine, and research associate at the Francis I. Proctor Foundation, UCSF School of Medicine, and sees patients in private practice at West Coast Retina Medical Group. They report no related financial interests.
___________________________
Supported in part by the Pacific Vision Foundation and San Francisco Retina Foundation.