By Kyle Smith, MD, Kendall K. Bicknell, MD, and He “Jack” Li, BA
Edited by Steven J. Gedde, MD
Download PDF
Cora Hardie* presented to our eye clinic with a six-month history of episodic bilateral vision loss. She described “blackouts” in both eyes that occurred several times a day, each lasting approximately 15 seconds. The 36-year-old told us that these episodes had been steadily increasing in frequency and seemed to be precipitated by standing up from a sitting position.
We Get a Look
Past ocular history. Her ocular history was remarkable for three episodes of iridocyclitis in the left eye starting two years earlier that had been managed elsewhere with topical steroids.
Past medical history. She had a long history of iron-deficiency anemia and had been complaining of unintentional weight loss and fatigue since age 25. At 33 years of age, she began experiencing chest pains and palpitations. At 34, she developed a recurring “burning pain”—and later, a periodic weakness—in her left arm. One month before we first saw her, she also noted a persistent sensation of “dizziness,” especially upon standing. During these syncope episodes—which she said lasted about 15 seconds—she would have to sit down and rest before continuing with her daily activities.
Her primary care provider had already investigated these complaints with a hepatitis panel, rapid plasma reagin (RPR) test, gonorrhea/chlamydia test, and multiple tests for thyroid-stimulating hormone (TSH) levels, all of which were unremarkable.
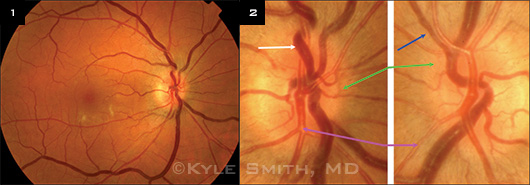
Initial examination. In her initial ophthalmologic examination, she had 20/20 uncorrected visual acuity in both eyes. Her confrontation visual fields and pupils were normal. She had asymmetric intraocular pressures of 13 mmHg in the right eye and 8 mmHg in the left. Her anterior segments were normal, with no evidence of anterior uveitis, although a few clumps of pigment on the anterior lens capsule of the left eye gave evidence of prior uveitis. Her funduscopic exam revealed moderately tortuous and dilated veins with areas of focal narrowing along the retinal arterioles in all four quadrants in both eyes. There were midperipheral hemorrhages in her left eye, and no retinal hemorrhages in her right eye. We noted moderate midperipheral cotton-wool spots in the right eye. We didn’t notice any signs of neovascularization in either eye. At this point, we suspected a vascular cause to her vision loss because a vascular insufficiency, exacerbated by activity, could explain the periodic presentation. Our differential diagnosis included vascular insufficiency, clotting disorder, ocular ischemic syndrome, carotid cavernous fistula, and migraine.
|
What's Your Diagnosis
|
 |
|
There were moderately tortuous and dilated veins, and focal narrowing along the retinal arterioles in the right eye (1), as well as in the left eye. (2) We also noted dilated tortuous veins (white arrow) in the right eye, venous beading in the left eye (blue arrow), and blurred disc margins (green arrows) and copper wiring (purple arrows) in both eyes.
|
Subsequent Evaluation
We suspected a systemic vascular or cardiac problem and referred her to our cardiology department for further evaluation.
The cardiologist noted a systolic murmur, a normal electrocardiogram (ECG), and a normal echocardiogram, and he concluded that her symptoms were not of cardiac origin. In light of her still-unexplained syncopal episodes, he referred her to nephrology.
The nephrologist found that she was not significantly hypotensive and documented another normal TSH and normal serum cortisol level. The nephrologist then referred the patient to neurology for further evaluation of the unexplained weakness in her left arm.
The neurology workup—which included an electroencephalogram (EEG), MRI of the cervical spine, and an anti-acetylcholine receptor antibody panel—was unremarkable.
Her persistent complaints then prompted a referral to rheumatology. Her workup there was remarkable only for an elevated erythrocyte sedimentation rate (ESR; 58 mm/hour) and C-reactive protein (26.1 mg/L).
Subsequent referral to endocrinology revealed no specific diagnosis or abnormalities other than the previously documented anemia.
The patient then experienced another episode of chest pain and went to the emergency department. A repeat ECG, cardiac enzymes, and a chest x-ray were all normal. Review of her medical record indicated that many of the physicians who saw her during this chain of referrals thought that her symptoms were likely nonorganic.
Finally, because of our continued concern for a vascular etiology, we referred her to the vascular surgery department. The vascular surgeon found that she was hypotensive (90/50 mmHg) and had a systolic ejection murmur radiating to the base of her neck. She also had bilateral carotid bruits and bilateral weak brachial and radial pulses. A carotid duplex ultrasound examination revealed severe stenosis (70-99 percent) of both common carotid arteries with concentric transmural thickening. Further ultrasound and computed tomographic angiogram (CTA) testing revealed diffuse arterial wall thickening involving the right vertebral artery, the thoracic and abdominal aorta, both common carotid arteries, both subclavian arteries, and both renal arteries.
Diagnosis and Treatment
These findings confirmed a diagnosis of Takayasu arteritis (TKA). After a short course of intravenous steroids, the patient left the hospital on oral prednisone and methotrexate.
When she returned for follow-up one month later, her episodes of transient visual loss had resolved and her other symptoms were markedly improved. Her funduscopic exam had returned to nearly normal. She will continue to follow up with vascular surgery and may eventually require elective carotid endarterectomy.
 |
|
ADDITIONAL SYMPTOMS. Scattered midperipheral hemorrhages (blue circles) in the left eye.
|
Pathophysiology
Takayasu arteritis is a chronic granulomatous arteritis that primarily affects the aorta and great vessels. The chronic inflammation associated with TKA produces endothelial damage in the great vessels, which leads to atherosclerosis and thickening of the arterial wall.1 Granulomatous inflammation of the carotid arterial wall can lead to chronic hemodynamically significant carotid stenosis, ocular hypoperfusion, and ocular ischemic syndrome (OIS).
OIS most commonly occurs as a result of occlusion of the common or internal carotid arteries, and only rarely from ophthalmic artery occlusion. Atherosclerosis is usually the cause of OIS, but other causes—such as fibrovascular dysplasia, carotid dissection, and TKA—have been reported.2 Symptoms may include loss of vision or of visual field, photophobia, and ocular or orbital pain.2 Anterior segment examination may reveal conjunctival and episcleral injection, scleral melting, iridocyclitis, cataract, and neovascular glaucoma. Posterior segment signs are those of chronic ischemia, including midperipheral retinal hemorrhage, cotton-wool spots, retinal vascular tortuosity or narrowing, retinal or choroidal neovascularization, and vitreous hemorrhage.
Clinical Considerations
Ms. Hardie presented to us with progressive episodic vision loss. She had suffered from years of unexplained systemic symptoms, including chronic fatigue, weight loss, weakness, dizziness, and palpitations, and, more recently, episodic vision loss. In retrospect, her episodes of recurrent iridocyclitis were likely the initial ophthalmologic manifestations of OIS. She saw many different specialists before the diagnosis was finally made 11 years after her symptoms began. During that time, she had at least 11 TSH levels drawn, all of which were normal. The absence of significant laboratory abnormalities led some doctors to conclude that her symptoms were nonorganic. Her delayed diagnosis is typical for TKA patients. A Mayo clinic study found that the median delay in diagnosis for patients under 40 years of age was 13.3 months, and 38.3 months for those over 40.3
Ophthalmologists should be aware of the signs and symptoms of OIS and should include TKA in the differential diagnosis, especially in younger patients who are less likely to have advanced atherosclerosis.
___________________________
* Patient name is fictitious.
___________________________
1 Alibaz-Oner F et al. Acta Cardiol. 2014;69(1):45-49.
2 Terelak-Borys B et al. Med Sci Monit. 2012;18(8):RA138-144.
3 Schmidt J et al. Mayo Clin Proc. 2013;88(8):822-830.
___________________________
Dr. Smith is an associate professor of ophthalmology and Dr. Bicknell is an ophthalmology resident at the Scott & White Eye Institute in Temple, Texas. Mr. Li is a medical student at Texas A&M Health Science Center College of Medicine in Temple, Texas. The authors report no related financial interests.