By Niranjan Manoharan, Patrick B. Hopen, MD, and Wanda M. Martinez, MD, PhD
Edited by Steven J. Gedde, MD
Download PDF
Andy Jackson* was a 30-year-old man who had never had eye problems before. But after eight days of pain, redness, photophobia, and mild blurry vision in his right eye, he went to the emergency room. He told the ER staff that he was HIV positive and that he was on highly active antiretroviral therapy. When the ER staff reviewed his medical records, they found that his viral load was undetectable at his last clinic visit.
On examination in the ER, Mr. Jackson’s visual acuity was 20/20- in each eye at near. The anterior segment exam of the right eye showed 2+ conjunctival injection, 2+ anterior chamber (AC) cells (without keratic precipitates or synechiae), and trace anterior vitreous cells. The remainder of the eye exam was normal.
 |
|
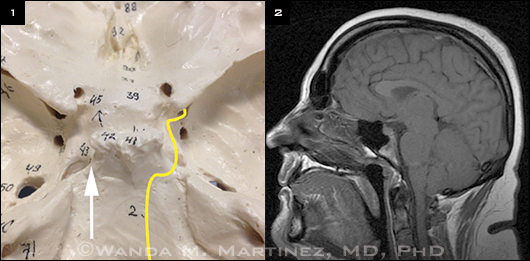
Critical details. (1) Cranial nerve VI (yellow line) negotiates a 90-degree bend at the apex of the petrous bone (white arrow), then travels under the petroclinoid ligament and horizontally along the internal carotid artery into the cavernous sinus. (2) Intracranial hypotension on MRI, showing downward displacement of the basal cisterns and cerebellar tonsils.
|
Full Workup
Mr. Jackson was prescribed prednisolone acetate drops every two hours and daily dilating drops for his anterior uveitis, and a workup was initiated. This included a complete blood count as well as the following tests: angiotensin-converting enzyme, erythrocyte sedimentation rate, fluorescent treponemal antibody absorption (FTAABS), HLA-B27, lysozyme, Quanti-FERON tuberculosis gold (QTB), and rapid plasma reagin (RPR).
Per the protocol of our institution’s infectious disease clinic, Mr. Jackson’s RPR and QTB had been checked the previous year; at that time, the results were negative.
Mr. Jackson was instructed to follow up at our uveitis clinic.
Problem Solved?
Five days later, Mr. Jackson reported complete resolution of his symptoms. His visual acuity was stable, his intraocular pressure (IOP) was normal, and there were trace AC cells in the right eye. No other pathology was evident.
However, results of the lab work revealed positive RPR and FTA-ABS, and he was admitted to the hospital. A lumbar puncture (LP) was performed. Although the procedure was more traumatic than is usual and left Mr. Jackson with a bad headache, it revealed a normal opening pressure, normal glucose and protein levels, a normal white blood cell count, and a negative Venereal Disease Research Laboratories (VDRL) test.
In addition, he tested negative for herpes simplex virus, Epstein-Barr virus, and cytomegalovirus. Neuroimaging was negative for intracranial pathology.
Mr. Jackson was sent home with an intravenous line to complete a 14-day course of IV penicillin on the basis of his converted RPR result for syphilis. He continued with his prednisolone drops and the dilating drop.
Double Trouble
Soon after his discharge, Mr. Jackson developed eye troubles again. He now noticed diplopia with right gaze and returned to our uveitis clinic.
At this point, Mr. Jackson’s visual acuity was 20/25+2 in his right eye and 20/20 in his left. His pupils reacted briskly with no afferent pupillary defect. Cover testing in primary gaze revealed a 15 prism diopter (PD) right esotropia, which increased to 25 PD in right gaze. The motility exam revealed a 40 percent abduction deficit in the right eye. The rest of the ocular movements in both eyes were full. The anterior segment exam revealed no cells or flare, and the posterior segment exam was unremarkable.
Pinning It Down
Given Mr. Johnson’s age, our differential diagnosis focused on acute abducens palsy, or sixth nerve (CNVI) palsy. In young adults, the most common causes of a CNVI palsy include brain lesions, idiopathic intracranial hypertension, meningitis, and multiple sclerosis,1 none of which fit this case.
We were especially concerned about the possibility of neurosyphilis in our patient, given his positive FTA-ABS and RPR results. However, in reported cases of CNVI palsy due to neurosyphilis, patients presented with abnormal serologic testing of cerebrospinal fluid (CSF)2—and Mr. Jackson’s CSF VDRL was normal. Viral infection was also unlikely, given the lack of a viral prodrome in our patient’s history. Moreover, Mr. Jackson’s blood pressure was under control, and his hemoglobin A1c level was within normal limits.
Given Mr. Jackson’s LP and subsequent headache, we quickly considered the diagnosis of a post-LP abducens nerve palsy.
Discussion
Cranial nerve palsies are well-documented complications of LP. The procedure can cause leakage of CSF from the dural puncture site, which produces intracranial hypotension and, in turn, traction on the cranial nerves. Of all post-LP palsies, CNVI palsies are the most common, given the nerve’s long course and its sharp bend around the petrous bone3 (Fig. 1).
Other procedures that can cause CN palsies include neuraxial anesthesia, contrast myelography, intrathecal glucocorticoid injections, and ventriculoperitoneal shunts.4
Incidence. The incidence of post-LP CNVI palsy ranges from 1 in 800 with 16-gauge needles to 1 in 5,800 with 22-gauge needles.5
Symptoms. Patients present with binocular horizontal diplopia that worsens in far gaze and in the direction of the palsy. Nearly all reported cases begin with a headache, and the diplopia occurs four to 14 days after the puncture.6
Use of imaging. Magnetic resonance imaging (MRI) is useful in ruling out other causes of CNVI palsies. Characteristic findings on MRI to suggest a post-LP palsy are related to intracranial hypotension (Fig. 2), such as small ventricles, meningeal enhancement, downward displacement of brain stem, and subdural fluid collection.
It has been suggested that intracranial hypotension caused by CSF leakage can lead to compensatory vasodilation or tearing of small meningeal vessels. This can lead to the diffuse postgadolinium meningeal enhancement and subdural fluid collection seen on MRI.
Management and Prognosis
Conservative treatment. Several strategies are aimed at restoring CSF volume to avoid symptoms and/or signs of intracranial hypotension. These include having the patient stay in a recumbent position as well as recommending supportive treatments such as oral/intravenous hydration, high oral caffeine intake, and high salt intake.
Blood patch. Epidural blood patching is the established treatment for post-LP headache, especially when conservative measures fail. Infusion of 10 to 20 mL of autologous blood into the epidural space causes tamponade of the dural leak, subsequent fibrin deposition, and scar formation. This will thereby prevent further CSF leakage, intracranial hypotension, and cranial nerve traction. There is some evidence that blood patching, when performed within 24 hours of the onset of a cranial nerve palsy, can lead to partial improvement or earlier resolution of symptoms.4 Based on this evidence, epidural saline infusions have also been advocated.
Long-term treatment. If the CNVI palsy persists, prisms or strabismus surgery may be required.
Prognosis. In more than 80 percent of cases of CNVI palsy, spontaneous recovery occurs within two to eight months. Palsies lasting longer than eight months are likely to be permanent. However, improvement has been reported up to the 12-month mark.4
Final Thoughts
An appropriate workup for uveitis should include an assessment of infectious causes, even if a prior infectious workup has been negative. In addition, post-LP abducens palsies should be considered in the post-LP differential diagnosis of acute diplopia.
Two months after the onset of diplopia, Mr. Jackson reported no remaining symptoms. He was orthophoric in primary gaze, and there was intermittent esotropia in extreme right gaze. He was lost to follow-up thereafter.
___________________________
* Patient’s name is fictitious.
___________________________
1 Peters GB III et al. Ophthalmology. 2002;109(10):1925-1928.
2 Slavin ML et al. Arch Ophthalmol. 1992;110(3):322.
3 Bechard P et al. Can J Anaesth. 2007;54(2):146-150.
4 Niedermüller U et al. Clin Neurol Neurosurg. 2002;104(1):61-63.
5 Thömke F et al. Neurology. 2000;54(3):768-769.
6 Quraishi SA. MedGenMed. 2005;7(4):16.
___________________________
Mr. Manoharan is a medical student, Dr. Hopen is an ophthalmology resident, and Dr. Martinez is an assistant professor of ophthalmology; all are at the Medical College of Wisconsin in Milwaukee. The authors report no related financial interests.