By Priscilla Luke, MD, James C. Pitts, MD, and Wei Li, BS
Edited by Steven J. Gedde, MD
Download PDF
Over the past month, Samuel Brook* had been treated as an outpatient for panuveitis in his right eye. Mr. Brook wasn’t a complainer; working construction jobs in the California desert all his life had taught him not to sweat the small things. He had been through a lot in the past year and his vision kept getting worse. Now, at the urging of his outpatient ophthalmologist, this 54-year-old Caucasian man was at the ER.
We Get a Look
Mr. Brook arrived at the ER on a Friday night. The on-call resident measured the vision in his right eye as hand motion at 1 foot. The resident also noted that Mr. Brook had an IOP of 29 mmHg in his right eye, even though he had been using topical and oral IOP-lowering medications—Combigan (brimonidine/timolol) and Diamox (acetazolamide)—prescribed by the outside ophthalmologist. He also was using topical Pred Forte (prednisolone acetate). Slit-lamp exam revealed a fixed pupil and a 4.5-mm hypopyon with fibrinoid aqueous in his right eye. B-scan ultrasound of the right eye revealed increased reflectivity of the vitreous but no significant vitreous debris. Vision and exam of the left eye were normal.
His medical history. Good health had been the norm for most of Mr. Brook’s life. His only eye problem had occurred more than 20 years ago when he experienced bilateral blurry vision for two days and was diagnosed with reactive arthritis (formerly Reiter’s syndrome). His vision spontaneously returned to normal and had not bothered him again until this year.
In the past few months, problems seemed to be piling up for Mr. Brook. A crush injury to his foot resulted in hospitalization for osteomyelitis. In addition to that, two lung masses were found on his chest x-ray. Positron emission tomography (PET) scans showed hypermetabolic activity of the larger lung mass, and his primary doctor considered it suspicious for cancer. He was seen by a pulmonologist and a cardiothoracic surgeon. The location of the masses wasn’t amenable to needle biopsy, so he was scheduled for excisional biopsy. While awaiting this biopsy, he began having trouble with the vision in his right eye—trouble that ultimately brought him to our ER.
Early differential diagnosis. Mr. Brook’s history and exam yielded an extensive differential diagnosis. A severe panuveitis might have been undertreated as an outpatient; the limited records that we saw for him suggested that a standard panuveitis workup was still needed. His recent osteomyelitis could be a source for endogenous endophthalmitis. Additionally, his lung nodules raised the specter of metastatic disease to the eye. Although we normally might tap and inject an eye to rule out endophthalmitis, we were concerned that, in Mr. Brook’s case, this could result in dissemination of possible metastatic disease. With the above considerations in mind, we had the patient admitted for further evaluation of his lung lesions and a workup for infection and panuveitis.
The Workup
The initial lab workup included a complete blood count (CBC), basic metabolic panel (BMP), and tests for erythrocyte sedimentation rate and C-reactive protein (ESR/CRP), angiotensin-converting enzyme (ACE), and lysozyme, which all returned within normal limits. Blood cultures for bacteria and fungi were drawn and remained negative. Autoimmune workup was positive for HLA-B27; however, testing for antinuclear antibody (ANA), rheumatoid factor (RF), perinuclear antineutrophil cytoplasmic antibodies (p-ANCA), cytoplasmic antineutrophil cytoplasmic antibodies (c-ANCA), and HLA-A29 revealed nothing positive. Infectious studies for syphilis, tuberculosis, human immunodeficiency virus (HIV), cytomegalovirus (CMV), herpes simplex virus (HSV-1 and -2), varicella-zoster, Bartonella, Toxoplasma, Toxocara, and Lyme disease were negative.
MRI did not reveal any evidence of metastasis to the brain or orbits.
We decided to obtain samples from the anterior chamber and vitreous. One of the aqueous samples stained positive for gram-positive cocci but did not grow any organisms; given that all other samples remained negative, the possibility of contamination was discussed. Staining and culture of all vitreous samples remained negative for bacteria and fungi. Cytology of samples revealed no malignant cells.
While waiting for these culture results, Mr. Brook underwent multiple rounds of intravitreal injections of vancomycin and ceftazidime. When cultures failed to reveal organisms, his topical steroid therapy was increased, and systemic steroid therapy was initiated. Initially, his IOP trended downward, but within the week became progressively elevated despite maximal medical therapy. After Mr. Brook had an Ahmed valve implanted, his IOP returned to normal, and he was discharged for further outpatient workup, still without a definitive diagnosis.
 |
|
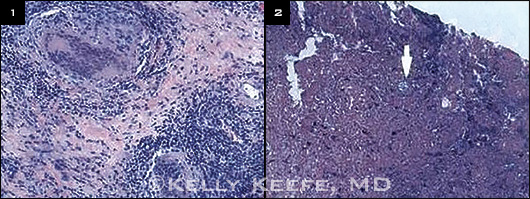
H&E. (1) Granulomatous inflammation with multinucleated giant cells. (2) Double-walled coccidioidomycosis organism (arrow), with endospores (bubbles) in it.
|
The Next Six Months
The patient was followed closely by glaucoma, uveitis, and retina specialists, as well as by rheumatology over the next six months. Despite the addition of azathioprine and, eventually, adalimumab by rheumatology for presumed autoimmune disease, progressive inflammation in the patient’s right eye obstructed his tube shunt. A second tube shunt, a vitrectomy with lensectomy, and eventually cyclophotocoagulation were unsuccessful in decreasing inflammation or reducing IOP. Vitreous samples taken during the vitrectomy again remained negative on bacterial and fungal cultures.
After six months of severe pain and poor vision despite the surgeries, Mr. Brook elected to undergo enucleation of his right eye. Initial pathologic evaluation of the globe returned a diagnosis of endophthalmitis; however culture of the globe revealed mold. The globe then underwent additional staining, which revealed giant cells, caseous granulomatous inflammation teeming with round cocci organisms, and double-walled organisms.
Cultures confirmed the diagnosis of coccidioidomycosis panophthalmitis secondary to Coccidioides immitis.
Discussion
Coccidioidomycosis is a relatively common systemic disease, especially in the southwestern United States and Mexico. Though a majority of individuals remain asymptomatic, approximately 40 percent develop a pneumonia-like syndrome. Less than 1 percent of patients develop disseminated disease, which most commonly presents as a soft tissue, bone, or central nervous system infection. Although coccidioidomycosis can affect any adnexal structure, the most common intraocular site is the uvea.
Diagnosis. The diagnosis has traditionally been based upon culture, stains, and serology. Coccidioides immitis and C. posadasii grow on many bacterial and fungal media and stain with hematoxylin-eosin (H&E), potassium hydroxide, periodic acid–Schiff (PAS), calcofluor white, and Gomori methenamine silver. Current serological tests tend to have good sensitivity and specificity, and advanced testing, including evaluation of the enzyme-linked immunosorbent assay (ELISA) and polymerase chain reaction (PCR) are undergoing further study.1 Intraocular coccidioidomycosis may have negative fungal cultures and serological studies, with ophthalmologists therefore relying primarily upon direct microscopy of specimens for diagnosis.2 In our case, the organisms were not noted on the original H&E stains and required a PAS stain for better visualization.
The disease has been reported to mimic other infections and neoplasm.
Treatment. Treatment options vary depending on the level of intraocular involvement, the extent of disseminated disease, and the immune status of the patient. If active disease is found with only ocular involvement, fluconazole (400-800 mg/day) either orally or intravenously is considered first-line treatment. For more disseminated disease, intravenous amphotericin B (0.5-1.0 mg/kg/day) is commonly the treatment of choice.3 Because intravenous amphotericin B has poor ocular penetration, it may be necessary to administer it intravitreally as well (1.5 µg/0.1 cc); however, retinal toxicity is not uncommon, so these patients must be followed closely. In addition to treatment with amphotericin B, these patients require subsequent long-term fluconazole treatment in order to eradicate the infection.
Follow-up
Mr. Brook is undergoing systemic antifungal treatment with fluconazole at the direction of an infectious disease specialist. He awaits excisional biopsies of his lung masses and continues to maintain good vision in his left eye.
___________________________
* The patient’s name is fictitious.
___________________________
1 Ampel NM. F1000 Med Rep. 2010;2:2. doi:10.3410/M2.
2 Vasconcelos-Santos DV et al. Ophthalmology. 2010;117(9):1839-1842.
3 Galgani J. Manifestations and Treatment of Extrapulmonary Coccidioidomycosis. www.uptodate.com. Accessed Sept. 10, 2014.
___________________________
Dr. Luke is an assistant professor of ophthalmology, Dr. Pitts is a senior resident in ophthalmology, and Mr. Li is a senior medical student at Loma Linda University in Loma Linda, Calif. They report no related financial interests.