By Yasha S. Modi, MD, Catherine Cukras, MD, PhD, Philip J. Rosenfeld, MD, PhD, and Audina M. Berrocal, MD
Edited by Steven J. Gedde, MD
Download PDF
Carlos Santiago,* a 5-year-old boy from Colombia, became worried when he suddenly experienced painless loss of vision and the appearance of dark shadows in his left eye. Even so, he initially kept his observation to himself, not wanting to ruin his family’s long-awaited vacation in Miami. Finally, after three days passed without any improvement in his vision, he told his mother, who rushed him to our ophthalmologic emergency room.
Mrs. Santiago reported that Carlos had always had blurred vision and had struggled to read the small letters at the doctor’s office. The year before, at home in Colombia, he had two similar episodes of sudden-onset vision loss with shadows in his right eye; each time, his vision spontaneously recovered over the course of 10 to 15 days. This was the first time, however, that he had any trouble with his left eye. Carlos confirmed his mother’s report. Upon further questioning, he denied having any difficulty seeing at night.
We Get a Look
Carlos’ general medical history was unremarkable. He had been a healthy baby, born at full term, and he continued to develop appropriately. He had not had any recent illnesses, and his vaccinations were all up to date per his mother’s accounting. He was not taking any medications or vitamins.
On examination, Carlos was in no apparent distress. A general survey of his skin, face, and body did not reveal any dysmorphic features. His best-corrected visual acuity (BCVA) was 20/70 and 5/200 in the right and left eye, respectively. There was no afferent pupillary defect, and his intraocular pressure (IOP) was within normal limits. We noted no nystagmus, and his ocular motility was full.
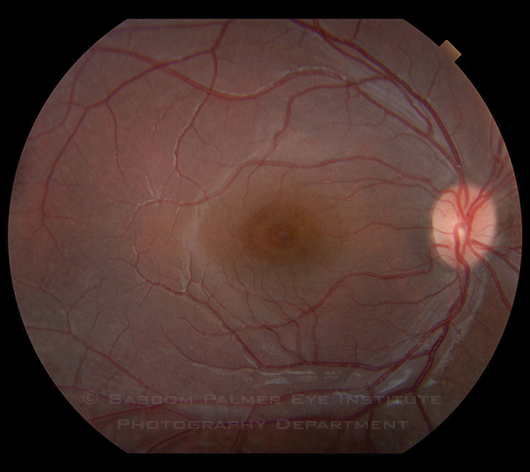
The slit-lamp examination was unremarkable except for 4+ pigmented cells in the anterior vitreous of the left eye. The fundus exam of the left eye was obscured by dense vitreous hemorrhage; that of the right eye (Fig. 1) revealed an elevated fovea with cystic changes and peripheral vitreous veils. An ultrasound of the left eye identified vitreous and subhyaloid hemorrhage without retinal detachment. We also noted macular thickening and multiple sites of vitreoretinal adhesions.
|
What's Your Diagnosis?
|
 |
|
The fundus examination of the right eye revealed an elevated fovea with cystic changes and peripheral vitreous veils.
|
Making the Diagnosis
At this point, it was apparent that Carlos had bilateral foveal thickening with likely recurrent episodes of vitreous hemorrhage. Given his age and these features, our differential diagnosis was highly focused. While enhanced S-cone syndrome (Goldman-Favre syndrome) and retinitis pigmentosa have overlapping features with this presentation, Carlos had recurrent vitreous hemorrhage without nyctalopia, making these diagnoses unlikely.
Additionally, while similar foveal changes can be seen in autosomal dominant cystoid macular edema or in the retinopathy related to the versican (VCAN) gene, as with Wagner syndrome, it would be rare for a patient to have concurrent vitreous hemorrhage. Recurrent vitreous hemorrhage in a young child also puts retinopathy of prematurity in the differential, but Carlos’ history of being carried to term and the presence of foveal findings were not consistent with this diagnosis.
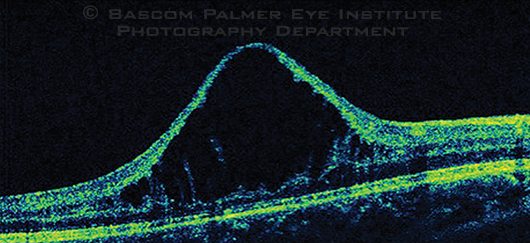
Further questioning revealed that Carlos had an uncle who had had very poor vision since birth. At this point, we obtained an OCT of Carlos’ right eye (Fig. 2). Given the bilateral foveal schisis, vitreous veils, recurrent vitreous hemorrhage, absence of nyctalopia, and positive family history, we diagnosed Carlos with X-linked retinoschisis (XLRS).
 |
|
Another Look. An OCT of the patient’s right eye was obtained to better characterize the foveal abnormality.
|
Discussion
Although XLRS is seen almost exclusively in males, there are a few case reports of females presenting with the disease. The incidence is estimated at 1:5,000 to 1:25,000.1
Presentation. The average age at diagnosis is between 4 and 6 years, with the earliest presentation in the literature occurring at 3 months.1 Classically, a school-aged boy is brought to a physician’s attention after it becomes clear that the child is having difficulty reading or he fails a vision screening. In approximately 10 percent of patients, a more precipitous decline in vision is the presenting complaint.
On examination, the pathognomonic finding is foveal schisis, which occurs in 100 percent of patients. Fifty percent of patients have peripheral retinoschisis, which is most commonly localized to the inferotemporal retina. Many patients have accompanying vitreous veils, which represent membranous remnants from the schisis cavity.
Genetics and pathogenesis. The defective gene is retinoschism 1 (RS1; formerly known as XLRS1), with more than 150 mutations reported that result in the XLRS phenotype. The gene encodes the protein retinoschisin, a discoidin domain family member thought to be important for cell adhesion and cell-to-cell interaction. The disruption of retinoschisin likely causes dysfunctional intraretinal adhesion and resultant schisis.
Although the splitting was originally thought to occur in the nerve fiber layer, high-resolution OCT has localized the cystoid spaces to deeper layers of the retina, most commonly in the inner nuclear layer.2 The pathogenesis of the foveal schisis is not completely known, but it is probably due to a dysfunction of retinoschisin and the resultant impact on synaptic integrity during foveal development.3
Complications. Vitreous hemorrhage, a common complication in XLRS, occurs as unsupported blood vessels in the thin inner retinal schisis cavity are damaged (either spontaneously or by minor trauma). Additional complications include hemorrhage into the schisis cavity, expansion of the schisis cavity into the macula, and combined schisis/retinal detachments, which require vitreoretinal surgery.
Management. Treatment of the foveal schisis is limited, with mixed results reported with carbonic anhydrase inhibitors.4 As the patient ages, however, there is collapse of cysts and evident retinal atrophy. BCVA is reduced in childhood; while it is not completely stationary, it declines modestly through life, barring a complicating event. Gene transfer therapy has been performed in mice deficient in RS1 via delivery of an adenovirus vector, with successful expression of retinoschisin and normalization of retinal anatomy and function.5 Human studies are currently lacking, but this proof-of-concept study suggests a role for gene therapy in humans with XLRS.
Back to Our Patient
Fifteen days after we initially saw Carlos, the vitreous hemorrhage cleared. A fundus exam of the left eye revealed spokelike foveal schisis that mirrored that seen in the right eye. Additionally, a shallow inferotemporal peripheral retinoschisis cavity was noted along with inferior vitreous veils. An electroretinogram showed the classic electronegative dark-adapted waveform seen in XLRS (selective reduction of the b-wave with relative preservation of the a-wave amplitude). Genetic testing confirmed the diagnosis by identifying a mutation in the RS1 gene.
Summary
XLRS is a rare disorder affecting young boys and is defined clinically by bilateral foveal schisis. Although complications may be treated to prevent severe visual loss, the foveal schisis progresses to retinal atrophy. As the disease results from single-gene mutations, gene therapy may eventually offer a treatment modality for these patients.
___________________________
* Patient’s name is fictitious.
___________________________
1 Tantri A et al. Surv Ophthalmol. 2004;49(2):214-230.
2 Gregori NZ et al. Br J Ophthalmol. 2009;93(3):373-378.
3 Takada Y et al. Invest Ophthalmol Vis Sci. 2004;45(9):3302-3312.
4 Genead MA et al. Arch Ophthalmol. 2010;128(2):190-197.
5 Zeng Y et al. Invest Ophthalmol Vis Sci. 2004;45(9):3279-3285.
___________________________
Dr. Modi is a resident in ophthalmology, Dr. Rosenfeld is professor of ophthalmology, and Dr. Berrocal is associate professor of clinical ophthalmology; all are at Bascom Palmer Eye Institute. Dr. Cukras is a retina fellow at the National Eye Institute. The authors report no related financial interests. They would like to thank Paul A. Sieving, MD, PhD, director of the NEI, for his guidance and support.