Download PDF
Katie Wilson,* a healthy 14-year-old girl, was in gym class when she was struck in the right eye with a tennis ball and suffered immediate loss of vision. She was promptly referred to us for evaluation of her ocular trauma and associated vision loss. Katie’s previous ocular history included a myopic refractive error, with both eyes achieving 20/20 vision with –3.75 D of spherical correction.
We Get a Look
When we initially examined Katie, her visual acuity (VA) was hand motion in the right eye and 20/20 in the left. The pupillary exam revealed a sluggish reaction to light in the right eye but no afferent pupillary defect. Ocular motility was normal. Her intraocular pressure (IOP) was mildly elevated in the right eye at 22 mmHg; it was 15 mmHg in the left eye.
The slit-lamp exam of the right eye revealed a clot in the superior angle and blood on the endothelium with 3+ circulating red cells. There was a small (less than 1 mm) layered hyphema inferiorly, no visible iris dialysis, and no phacodonesis. The fundus exam showed neither commotio retinae nor any peripheral retinal pathology.
We treated the injured right eye with prednisolone acetate 1 percent and cyclopentolate 1 percent drops, four times and two times daily, respectively, and gave her standard posthyphema activity instructions.
|
What's Your Diagnosis?
|
 |
|
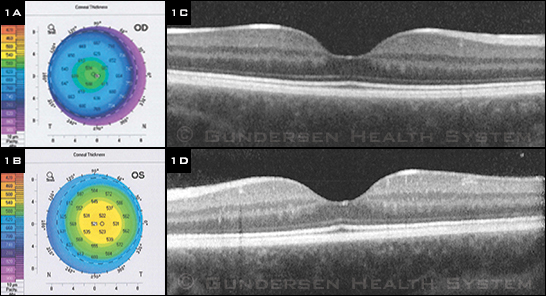
(1A, 1B) Postinjury scans showing corneal pachymetry of the right and left eyes, with (1C, 1D) corresponding macular OCT scans.
|
We Dig Further
The next day, Katie’s uncorrected VA had improved to 20/25 in her right eye. The IOP in this eye was now 29 mmHg, and she was started on Combigan (brimonidine/timolol) drops twice daily. She was acting very much like a typical hyphema patient in every regard—but her vision intrigued us.
At her next visit, after the weekend, the refraction was plano in her right eye (20/25) and –3.75 D in her left (20/20)—apparently, she was newly anisometropic. Her refractive error was significantly overcorrected in the right eye by her original prescription (–3.75 D in both eyes).
Eleven days later, her hyphema and ocular hypertension had resolved, and we elected to cycloplegically refract the left eye as well to make sure she wasn’t being overcorrected in both eyes. The result was +0.50 D in her right eye (20/30) and –3.50 D in her left (20/25). When asked, Katie said that before the injury, she definitely needed her contacts in both eyes to see well. If this was true, what had given her a 4-D hyperopic shift in her right eye?
Differential Diagnosis
At this point, we considered possible causes for a hyperopic shift. The refractive state of the eye is determined by several anatomic structures: the optical power of the cornea, the optical power of the lens, the anterior chamber depth, and the axial length. Conditions that shorten the distance between the cornea and posterior pole may induce hyperopia, such as external globe compression by a mass. Although progressive cataract formation usually produces a myopic shift, a drift toward hyperopia is occasionally seen, especially with cortical cataracts. Posterior subluxation of the lens with deepening of the anterior chamber can produce a hyperopic shift. Additionally, reduction in the curvature of the cornea decreases its effective power and induces hyperopia.
Investigating the Shift
An OCT of the right macula was normal (Fig. 1). Corneal topography revealed K1/K2 measurements of 39.0/39.5 D in the right eye and 42.0/42.6 D in the left eye immediately following the injury. The central corneal thickness was 591 µm in the right eye and 519 µm in the left eye. Axial length measurements were 24.77 mm and 24.55 mm in the right and left eyes, respectively.
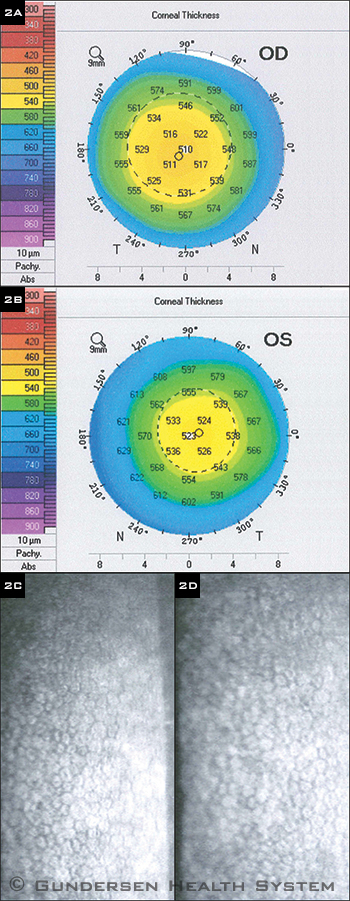
Katie was seen in clinic two months later for a recheck with gonioscopy. She said she needed her contacts again in both eyes in order to see. Her cycloplegic refraction revealed –4.25 D in her right eye (20/25) and –3.75 D in her left (20/25). Corneal pachymetry and specular microscopy studies were obtained; at this point, the diffuse thickening previously seen in the right cornea had resolved (Fig. 2). Central corneal thickness was 510 µm, and the K1/K2 measurements increased to 42.0/42.6 D in the right eye.
 |
|
RESOLUTION. (2A, 2B) Corneal topography of the right and left eyes, with (2C, 2D) corresponding specular microscopy. Note the decrease in corneal thickness in the right eye and the normal corneal endothelial cells on specular microscopy.
|
Discussion
Blunt ocular trauma results in a range of sequelae, including acute corneal edema, hyphema, cataract formation, lens subluxation, vitreous hemorrhage, choroidal and retinal rupture or detachments, commotio retinae, traumatic optic neuropathy, and globe rupture. Vision loss may also occur, with a spectrum of severity ranging from minimal transient vision loss to permanent blindness.
Traumatic hyphema is a well-known consequence of blunt eye trauma, with a reported median annual incidence of 17 per 100,000 population.1 Several complications can arise from traumatic hyphemas, including increased IOP, peripheral synechiae, corneal bloodstaining, glaucoma, and accommodative impairment.2 Elevations in IOP, which may be transient, are seen in one-third of all hyphema patients and are frequently managed with topical beta-adrenergic antagonists or alpha-2 adrenergic agonists.3 Although hyphemas are a common anterior segment complication of blunt eye trauma, the cornea may also be affected.
Corneal responses to blunt ocular trauma have not been well documented in the literature. Blunt injuries can result in corneal abrasions, acute corneal edema from endothelial cell dysfunction, and Descemet membrane tears.4 Additionally, blunt trauma to the eye can induce corneal astigmatism, particularly in cases of trauma resulting from small, hard objects.5 Unfortunately, there are no long-term studies to determine if these corneal changes are permanent or—as in Katie’s case—transient.
Back to Our Patient
The blunt ocular injury seen in our patient resulted in a transient hyperopic shift. Corneal pachymetry and topography of the right eye showed a transient thickening and flattening of the cornea immediately following the injury, which had resolved at the two-month follow-up visit. This trauma-induced hyperopic shift might have resulted from corneal stromal thickening without visible edema secondary to transient endothelial cell dysfunction.
To our knowledge, this is the first report of such findings in a pediatric patient with blunt trauma to the eye.
___________________________
* Patient’s name is fictitious.
___________________________
1 Agapitos PJ et al. Ophthalmology. 1987;94(10):1238-1241.
2 Crouch ER Jr, Crouch ER. J Pediatr Ophthalmol Strabismus. 1999;36(5):238-250.
3 Walton W et al. Surv Ophthalmol. 2002;47(4):297-334.
4 Kanski J, Bowling B. Clinical Ophthalmology: A Systematic Approach. 7th ed. Philadelphia: Elsevier; 2011.
5 Akinci A et al. Cornea. 2007;26(5):539-542.