By Marco A. Gonzalez, MD, and Janet L. Davis, MD
Edited by Steven J. Gedde, MD
Download PDF
Ulysses Forgeron* first consulted us in July 2007, complaining of blurry vision in his right eye. The 48-year-old cook told us that his vision had become progressively worse over a two-month period. In addition, he said, a central “dark spot” in his vision in that eye had increased in size during the preceding month. Mr. Forgeron told us that he had experienced similar symptoms in his left eye in 2001 that had not resolved. He also noted occasional flashes and mild periorbital pain in his right eye.
We Get a Look
When we examined Mr. Forgeron, his BCVA was 20/400 in his right eye and 20/50 in his left without an afferent pupillary defect. His intraocular pressure was 18 mmHg in each eye. The anterior segment exam was notable for 1+ cells in the right eye and a deep and quiet chamber in the left eye.
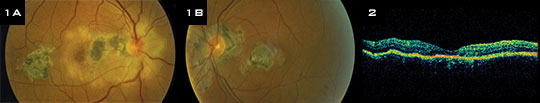
The dilated funduscopic examination revealed clear media. In the right eye, we noted a mildly blurred disc margin with a surrounding white chorioretinal infiltrate that extended into the central macula; this had variable areas of chorioretinal atrophy and hyperpigmentation (Fig. 1A). In the left eye, the disc margins were sharp; there was pronounced peripapillary atrophy and chorioretinal scarring as well as a variably pigmented macular scar (Fig. 1B). No active chorioretinal lesions were evident in the left eye.
Fluorescein angiography of the right eye revealed early hypofluorescence corresponding to areas of scarring with late hyperfluorescence around the borders. There was also early hyperfluorescence of the disc with late leakage. Optical coherence tomography of these lesions showed significant retinal thinning with subretinal hyperreflectivity (Fig. 2). We determined that Mr. Forgeron had active chorioretinitis in his right eye and healed chorioretinitis in his left.
|
What's Your Diagnosis?
|
 |
|
(1A) The right eye showed a white chorioretinal infiltrate in a peripapillary location. (1B) In the left eye, there was significant peripapillary chorioretinal scarring with a central macular scar. (2) An OCT of the right eye showed significant retinal thinning in the area corresponding to the infiltrate.
|
Differential Diagnosis
At this point, our differential diagnosis included infectious causes, such as toxoplasmosis, tuberculosis, or syphilis, and inflammatory causes, such as sarcoidosis and certain white dot syndromes. The latter category includes acute posterior multifocal placoid pigment epitheliopathy, multifocal choroiditis and panuveitis, and serpiginous choroiditis.
Pinning It Down
When we questioned Mr. Forgeron further, no other past medical history emerged. He denied having any recent illnesses and noted that he had emigrated from Haiti many years ago. The initial workup included a complete blood count and the rapid plasma reagin, fluorescent treponemal antibody absorption, and angiotensin-converting enzyme tests. Results were within normal limits. He did not test positive for HIV. But the tuberculin skin test (PPD) was positive with a negative chest x-ray, which raised suspicions of a serpiginous-like tuberculous choroiditis.1
Mr. Forgeron was placed on a nine-month regimen of quadruple antituberculosis therapy with isoniazid, rifampin, pyrazinamide, and ethambutol, which he completed. In addition, he was started on a tapering course of prednisone. The active retinitis subsequently resolved.
Two years later, in 2009, Mr. Forgeron was diagnosed with prostate cancer. In 2010, he returned with an active lesion in his left eye (Fig. 3) and a decision was made to treat him with oral prednisone and begin immunosuppression with mycophenolate mofetil. He was subsequently lost to follow-up and stopped refilling his prescriptions.
In December of 2011, he returned with active lesions in both eyes (Figs. 4A and 4B). He was restarted on immunosuppression, this time with prednisone and azathioprine. Mr. Forgeron has responded very well to this regimen, and his active lesions have resolved. He continues to follow up in the resident uveitis clinic without subsequent reactivation of his chorioretinitis.
 |
|
FOLLOW-UP. The disease can be tenacious, as our patient’s experience confirms. (3) Three years after initial treatment, he returned with an active lesion in the left eye. (4A, 4B) A year after that, he presented with active bilateral disease.
|
Discussion
Serpiginous choroiditis is a rare bilateral, chronic, and progressive inflammatory disease of unknown etiology that involves the retinal pigment epithelium, choriocapillaris, and choroid.2 Originally described and named “peripapillary chorioretinitis,” the condition has been known by a variety of names since its initial description, with the term “serpiginous choroiditis” entering the lexicon following Dr. Donald Gass’ use of it in 1987.
Incidence and pathogenesis. The disease affects healthy young-to-middle-aged adults, and it has no racial predilection. In most epidemiologic studies, serpiginous choroiditis constitutes less than 5 percent of all posterior uveitis.3 Studies have suggested myriad etiologies, with Herpesviridae and tuberculosis the most commonly proposed causes.
Symptoms and complications. Even though it tends to be a bilateral disease, serpiginous choroiditis commonly presents with unilateral symptoms of vision loss. Associated complications include choroidal neovascularization, vein occlusions, pigment epithelial detachments, cystoid macular edema, and optic disc neovascularization.
Diagnosis and Treatment
Diagnosis. Creamy choroidal infiltrates are the hallmark of active disease in serpiginous choroiditis, and they are seen with variably pigmented areas of scarring. Classically, the choroidal lesions appear initially in a peripapillary location and extend in an irregular “serpentine” fashion centrifugally. Active lesions usually resolve with or without treatment within weeks and leave an area of atrophy involving the RPE and choriocapillaris. Recurrences are common and usually extend from previous areas of atrophy.
On a fluorescein angiogram, active lesions and areas of atrophy will hypofluoresce early, with late hyperfluorescence occurring in the intermediate and late stages of the disease at the edges of the lesions and in areas of activity. These findings, although helpful, are not pathognomonic.
Findings are similar with indocyanine green angiography, although areas of hypofluorescence are often larger with ICG than are those seen clinically on fluorescein angiography. Hyperfluorescence is a common finding on ICG at active borders. Fundus autofluorescence can be used to track disease progression, as scarred areas devoid of functioning RPE will appear hypoautofluorescent, whereas active lesions are hyperautofluorescent.
Treatment. Most treatment regimens have consisted of initial steroid therapy for active lesions, followed by maintenance chronic immunosuppression with steroid-sparing therapy (such as azathioprine, mycophenolate, or cyclosporine) for at least six months following an acute episode.
The decision to pursue indefinite chronic steroid-sparing immunosuppression usually is made by weighing the risks of future vision loss and the patient’s comorbidities and balancing them against risks associated with chronic immunosuppression. In patients with a positive PPD, combined antituberculosis and immunosuppressive therapy appears beneficial.4
___________________________
* Patient’s name is fictitious.
___________________________
1 Gupta V et al. Ophthalmology. 2003;110(9):1744-1749.
2 Lim WK et al. Surv Ophthalmol. 2005;50(3):231-244.
3 Chang JH, Wakefield D. Ocul Immunol Inflamm. 2002;10:263-279.
4 Gupta V et al. Am J Ophthalmol. 2011;152(5):857-863.e2.
___________________________
Dr. Gonzalez is an ophthalmology resident and Dr. Davis is professor of ophthalmology; both are at the Bascom Palmer Eye Institute in Miami. The authors report no related financial interests.
Best of Grand Rounds
Grand Rounds: Cases and Experts From Across the Nation. At 3:45 on Monday afternoon, enjoy six memorable case reports. Nicholas J. Volpe, MD, who will be chairing this event, contacted several academic programs and invited them to present the most intriguing cases discussed at their grand rounds.
The six cases are as follows:
- “Battle of the Two,” presented by Michelle Y. Wang, MD *(3:47 p.m.)
- “It Is Not Adding Up,” presented by George N. Magrath, MD (3:58 p.m.)
- “Itchy Eyes and Vision Loss,” presented by Brian W. Toussaint, MD (4:09 p.m.)
- “Retinal Hemorrhage,” presented by John J. Chen, MD )4:20 p.m.)
- “Intraocular Foreign Body,” presented by Crandall E. Peeler, MD (4:31 p.m.)
- “Can’t See,” presented by Ehsan Rahimy, MD (4:43 p.m.)
When: Monday, Nov. 11, 3:45-5 p.m. Where: Room S406a. Access: Free.
|