Download PDF
Curtis Brown* started having episodes of painless, blurry vision in his right eye in 1989, the year he turned 32. Mr. Brown was diagnosed with right anterior uveitis, and he received short courses of topical steroids for periodic flare-ups. After eight years of recurrent anterior uveitis and its management, a significant cataract formed in his right eye. Cataract surgery was performed, and a posterior chamber IOL was inserted.
Although Mr. Brown’s vision cleared at this point, his symptoms returned in 2002. At that time, he developed a recurrence of his right anterior uveitis and presented with painless, blurry vision without redness or photophobia. Topical steroids were initiated, and his symptoms resolved. For the next five years, he took short, tapered courses of topical steroids and received several sub-Tenon injections for the recurrent anterior uveitis.
Glaucoma Develops
In 2007, at age 50, Mr. Brown, who is African-American, saw a glaucoma specialist for elevated intraocular pressure (IOP) and superior arcuate visual field defects in his right eye. The ophthalmologist diagnosed uveitic glaucoma and prescribed a topical beta-blocker, to be used twice a day. Mr. Brown’s left eye was normal without any glaucomatous changes.
A year later, the unilateral glaucoma had worsened: The IOP of Mr. Brown’s right eye peaked at 36 mmHg and remained in that range despite maximal medical therapy. Mr. Brown underwent the placement of an anterior chamber tube shunt with scleral patch graft in his right eye. Despite surgery, his IOP slowly rose above target, and he was started on timolol/dorzolamide drops twice a day in the right eye.
We Get a Look
In June of 2012, Mr. Brown had another flare-up of his anterior uveitis, and he was referred to our clinic.
When we saw him, Mr. Brown told us that he was taking two antihypertensive drugs and a cholesterol-lowering agent. In addition, he mentioned a recurrent history of fever blisters in his mouth. Mr. Brown’s best-corrected visual acuity (BCVA) was 20/40 in the right eye and 20/25 in the left. Both pupils were equally round and reactive, with no afferent pupillary defect. His confrontation visual field showed a small right superior arcuate defect, and motility was full bilaterally.
During the slit-lamp examination of the right eye, it was evident that the sclera and conjunctiva were noninjected and that diffuse stellate keratic precipitates (KPs) were present (Fig. 1). In addition, 2 to 3 cells/mm2 were noted in the anterior chamber, and no posterior synechiae were observed. Mr. Brown’s right iris was much lighter than his left iris and exhibited pigment loss diffusely (Figs. 2A, 2B). The slit-lamp exam of the left eye was within normal limits, apart from an early nuclear sclerotic cataract.
The funduscopic exam showed glaucomatous cupping (cup-to-disc ratio of 0.8) with a thin inferior rim, with a notch, in the right eye. There was no evidence of retinochoroiditis, vitritis, or previous chorioretinal scars. The left optic nerve was normal, with a cup-to-disc ratio of 0.3 and normal distribution of rim tissue.
|
What's Your Diagnosis
|
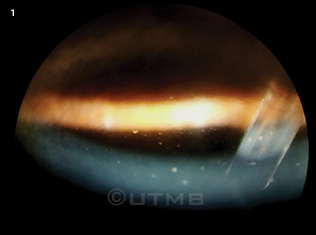 |
Diffuse stellate keratic precipitates were evident on the slit-lamp exam.
|
Differential Diagnosis
Considering Mr. Brown’s more than 20-year history of recurrent anterior uveitis without any conjunctival injection, the presence of iris heterochromia and diffuse stellate KPs, and his history of steroid use and unilateral glaucoma, we formulated a differential diagnosis that included Fuchs heterochromic iridocyclitis (FHI), toxoplasmosis, syphilis, uveitis associated with human leukocyte antigen (HLA) B27, and sarcoid-related uveitis. The differential also included uveitis linked to Herpesviridae: herpes simplex virus (HSV), varicella-zoster virus (VZV), and cytomegalovirus (CMV).
A detailed history and review of systems did not elicit anything suggestive for toxoplasmosis, HLA-B27–positive spondyloarthropathy, or sarcoidosis. Based on the history of recurrent fever blisters and clinical findings of anterior uveitis, Mr. Brown was empirically started on a topical prednisolone acetate taper, as well as 400 mg of oral acyclovir five times daily.
We also initiated a workup that included serum polymerase chain reaction (PCR) for CMV, immunoglobulin G (IgG) antibodies directed against CMV, fluorescent treponemal antibody absorption (FTA-ABS) test, HLA-B27, serum angiotensin-converting enzyme (ACE) level, and chest x-ray. Mr. Brown’s serum PCR for CMV was undetectable, and the anti-CMV IgG and FTA-ABS test results were negative. He did not have the HLA-B27 antigen, and his serum ACE levels were within normal limits. The chest x-ray did not reveal any problems.
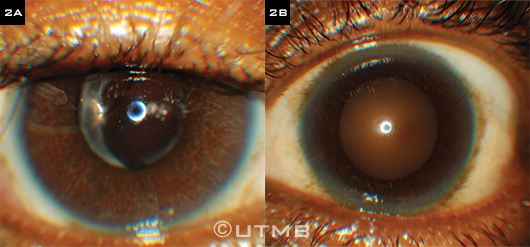 |
Critical Clue. Mr. Brown’s right iris (2A) was lighter than his left iris (2B).
|
Pinning It Down
At this point, our differential focused on HSV- and VZV-associated uveitis. However, despite a three-week course of full-dose acyclovir and topical steroid drop taper, Mr. Brown’s right unilateral anterior uveitis with stellate KPs persisted with minimal change from his baseline exam.
Because HSV- and VZV-related anterior uveitis typically respond to full-dose oral acyclovir and topical steroids, we now felt that those diagnoses were unlikely. And as the CMV lab results were negative, the possibility of CMV-related uveitis was diminished. Finally, because our patient didn’t exhibit any posterior synechiae, conjunctival injection, or change in presentation with empiric antiviral treatment, we ruled out herpesvirus and discontinued the oral acyclovir. In view of these findings and the exclusion of other possible diagnoses, we made the diagnosis of FHI.
Discussion
Fuchs heterochromic iridocyclitis is usually a unilateral iridocyclitis with characteristic stellate KPs and iris heterochromia. In dark-eyed patients, iris stromal atrophy causes the affected iris to appear lighter than the normal one. In individuals with light-colored eyes, however, the involved eye may be darker (heterochromia inversa) because iris atrophy exposes the pigment epithelium.
In 1906, Ernst Fuchs defined the syndrome as a triad of anterior uveitis, heterochromia, and cataract formation.1 The typical age of onset is 20 to 40 years of age, with men and women equally affected.2 The etiology of FHI is unclear. However, several studies have linked FHI to the rubella virus.3,4
Symptoms. Patients with FHI are generally asymptomatic, with only blurred vision or vitreous floaters from chronic inflammation. They may present with mild anterior chamber reaction with little or no ciliary injection or pain. Symptoms can include diffuse stellate KPs, iris atrophy with or without heterochromia, later-onset elevated IOP or glaucoma, and mild vitritis.
Diagnosis. FHI should always be considered in patients with glaucoma and uveitis. The diagnosis is primarily made by a detailed history and clinical exam. Analysis of aqueous humor for antibodies directed against herpesvirus and the rubella virus or viral-specific DNA can aid in the diagnosis.3,5
Management. Overall, FHI treatment consists of removing cataracts and controlling IOP. If glaucoma does not develop, then the prognosis is generally good. However, the management of uveitis and glaucoma related to FHI can be challenging: The uveitis in FHI typically doesn’t respond to topical corticosteroids, and although topical glaucoma medications may initially control the glaucoma, most cases of FHI-associated glaucoma are resistant to topical medications.2
Back to Our Patient
Mr. Brown’s uveitis has been stable, without subsequent flare-ups since June 2012. He continues to be followed by the glaucoma specialist, and his FHI-associated glaucoma has been stable without further progression.
___________________________
* Patient name is fictitious.
___________________________
1 Fuchs E. Z Augenheilkd. 1906;15:191-212.
2 Siddique SS et al. Surv Ophthalmol. 2013;58(1):1-10.
3 Quentin CD, Reiber H. Am J Ophthalmol. 2004;138(1):46-54.
4 Suzuki J et al. Graefes Arch Clin Exp Ophthalmol. 2010;248(10):1487-1491.
5 Cunningham ET Jr, Baglivo E. Am J Ophthalmol. 2009;148(4):479-481.
___________________________
Ms. Yari is a medical student, and Dr. Kapur is a cornea and external disease specialist; both are at the University of Texas Medical Branch at Galveston. The authors report no related financial interests.