Download PDF
Orbital cellulitis is a potentially sight- and life-threatening disease that tops the ophthalmology worry list. Add methicillin-resistant Staphylococcus aureus (MRSA) to the mix of potential causative bacteria, and the level of concern rises even higher. MRSA has become a relatively prevalent cause of ophthalmic infections; for example, one study showed that 89 percent of preseptal cellulitis S. aureus isolates are MRSA.1 And preseptal cellulitis can rapidly develop into the more worrisome condition of orbital cellulitis if not treated promptly and effectively.
Moreover, the community-associated form of MRSA (CA-MRSA) now accounts for a larger proportion of ophthalmic cases than health care–associated MRSA (HA-MRSA). Thus, many patients do not have the risk factors that would alert a physician that an otherwise unimpressive eyelid lesion could be the precursor of a serious drug-resistant infection.
Part 1 of “MRSA Ophthalmic Infection” (in last month’s EyeNet) provided an overview of current realities regarding the prevalence of and increasing threat posed by drug-resistant S. aureus. This month focuses on diagnosing and treating MRSA preseptal and orbital cellulitis, which has an atypical presentation and course.
|
Acute MRSA Cellulitis
|
 |
|
(1A) This 19-month-old boy presented with left periorbital edema and erythema five days after having been diagnosed in an ER with conjunctivitis and treated with oral and topical antibiotics. (1B) Axial CT image of the orbits with contrast shows lacrimal gland abscess and globe displacement.
|
CA-MRSA’s Link to Cellulitis
In studies looking at patients with ophthalmic MRSA in the Parkland Health and Hospital System in Dallas, 86 percent of those with preseptal cellulitis and/or lid abscesses had CA-MRSA. These studies also found that preseptal cellulitis was the most common ophthalmic MRSA presentation from 2000 to 2009,2,3 followed by conjunctivitis, corneal ulcer, endophthalmitis, and orbital cellulitis; and the average age of patients was 32.7 years (standard deviation [SD], 18.1 years). Why does CA-MRSA have such a strong predilection for causing cellulitis?
The answer appears to be that the CA form of MRSA is associated with a particular staphylococcal toxin known as Panton-Valentine leukocidin, which causes tissue necrosis and leukocyte destruction. This toxin, a major factor in the etiology of abscesses of the skin and eyelids, is rarely produced by other types of S. aureus bacteria, whether HA-MRSA or methicillin sensitive.
Oral Antibiotics for Preseptal Cellulitis
The following oral antibiotic regimens are appropriate choices for controlling mild to moderate CA-MRSA infections, such as preseptal cellulitis and dacryocystitis.
- Trimethoprim/sulfamethoxazole: loading dose of two double-strength tablets twice a day, then one tablet twice a day.
- Clindamycin: 450 mg three times a day. (Dr. Hwang advises watching for macrolide-inducible resistance, which has about a 50 percent incidence.)
- Minocycline (preferable to doxycycline): 100 mg twice a day.
- Linezolid: 600 mg twice a day. (Watch for myelotoxicity, and be aware that linezolid is extremely expensive, said Dr. Hwang.)
Plus:
- Rifampin: 300 mg twice a day for five days, in combination with one of the antibiotics listed above.
|
When to Suspect MRSA Orbital Cellulitis
Patients with orbital cellulitis commonly complain of pain when moving the eye, decreased vision, and limited eye movement. They may present with proptosis, an abnormal pupil, swelling of the eyelid and/or under the conjunctiva, and fever and discharge.
Orbital cellulitis is commonly caused by sinusitis or other nearby infections, trauma, or prior surgery. But the picture may be different when MRSA is the cause. “If we see the telltale signs and symptoms of orbital cellulitis in the absence of sinus disease, upper respiratory illness, or previous skin trauma, that raises a flag for potential MRSA orbital infection,” explained Vikram D. Durairaj, MD, at the University of Colorado in Denver. “Diffuse lid swelling with multiple areas of involvement, such as the lacrimal glands and extraocular muscles, also suggests a MRSA orbital infection,” said Dr. Durairaj, who is one of the coauthors of a recent paper that identified several distinctive features of atypical orbital cellulitis caused by MRSA.4
Dr. Durairaj’s team retrospectively analyzed the medical records of 15 patients with orbital cellulitis who were culture positive for MRSA. The patients, with a mean age of 31.9 years (range, 2-62 years; SD, 24.2 years), were managed by ophthalmic plastic surgeons between January 2006 and April 2009 at several institutions in the United States. The authors noted that this is the largest case series of MRSA-related orbital cellulitis published to date.
Characteristics of MRSA orbital cellulitis. In this study, the MRSA-associated orbital cellulitis most commonly presented as eyelid lesions with lid swelling (preseptal cellulitis) that progressed rapidly, as was seen in 14 of the 15 patients. Many of these patients stated that they first developed an eyelid lesion similar to a boil or stye, and the condition gradually worsened to cellulitis with numerous microabscesses along the lid margin. In a number of cases, these lesions were initially thought to be spider or insect bites on the eyelid.
None of the patients had a preceding upper respiratory infection, and only one patient had a history of eyelid or other ocular trauma. Paranasal sinus disease was uncommon, occurring in three of 15 patients. According to the authors, this finding is particularly significant for a pediatric population because prior studies have shown that orbital cellulitis in children is frequently associated with paranasal sinus disease; and it could have major implications for diagnosis and management of young patients.
Suspicious findings. Whenever a clinician sees a case of orbital cellulitis, he or she should have a high index of suspicion for MRSA, said Dr. Durairaj, but especially in endemic areas and in patients with lid swelling and the following characteristics:
Presence of
- Lacrimal gland abscesses
- Multiple orbital abscesses
Absence of
- Recent upper respiratory illness
- Prior periorbital trauma
- Adjacent paranasal sinus disease, especially in the pediatric population
“If the orbital infection has an unusual presentation, is not following the typical clinical course, and is getting worse, practitioners should not hesitate to escalate care by involving an oculofacial plastic and orbital surgeon,” Dr. Durairaj advised.
MRSA Treatment Pointers
- Stay up to date on what organisms are endemic to your area. If CA-MRSA is endemic, change your practice to cover it, especially when treating preseptal cellulitis to prevent orbital cellulitis.
- Save the agent of last resort—vancomycin—for serious MRSA infections such as orbital cellulitis.
- For mild to moderate infections, use older antibiotics that effectively cover CAMRSA.
- Use adequate dosing of appropriate antibiotics. Get in, hit hard, and get out.
- If you suspect MRSA-related orbital cellulitis, consider immediate surgical drainage of any focal abscess in addition to appropriate empiric antibiotic coverage.
|
Treatment for Ocular MRSA Cellulitis
Nip it in the bud. Given that Dr. Durairaj’s paper reported that rapidly progressing preseptal cellulitis was the primary predictor of MRSA orbital cellulitis, it’s important to intervene promptly. “Since Hib vaccination became routine, we may have become complacent about preseptal cellulitis,” said Preston H. Blomquist, MD, at University of Texas Southwestern Medical Center. (Haemophilus influenzae was formerly the most common cause of orbital cellulitis, the incidence of which has declined dramatically since the introduction of the Hib vaccine in 1990.) “This finding wakes us back up to the importance of monitoring our preseptal cellulitis patients closely. While it’s true that orbital cellulitis caused by MRSA doesn’t occur that often, you have to be prepared for the threat,” he said.
Preseptal cellulitis. Appropriate treatment for preseptal cellulitis in CA-MRSA endemic areas includes 1) empiric antibiotic coverage for CAMRSA and 2) incision and drainage of any lid abscesses, according to Dr. Blomquist. “Appropriate drainage is the definitive management of many skin and soft tissue infections and an important adjunct to antibiotic therapy in deep, closed-space infections,” he said.
Fortunately, CA-MRSA is susceptible to several antibiotics, including tetracyclines and aminoglycosides (see “Oral Antibiotics for Preseptal Cellulitis”). “One need not jump to vancomycin initially for nonsevere infections,” emphasized Dr. Blomquist, whose oral therapy for preseptal cellulitis is double-strength trimethoprim/sulfamethoxazole (two tablets twice daily), with or without rifampin. Beta-lactam antibiotics (e.g., penicillins and cephalosporins) alone for preseptal cellulitis should be avoided in CA-MRSA endemic areas; CA-MRSA also shows high levels of resistance to erythromycin and fluoroquinolones, he said. Clindamycin may also be considered. However, David G. Hwang, MD, at University of California, San Francisco, cautioned that macrolide-inducible resistance to clindamycin may be present in some geographic areas.
Dr. Blomquist said, “At Parkland Hospital here in Dallas, we get a lot of preseptal cellulitis presenting in the emergency room. Ophthalmologists don’t even see these cases because our protocol in the ER is to treat preseptal cellulitis with an antibiotic that also covers CA-MRSA. That’s because Dallas is endemic for it.”
Staff in the emergency room often have a better handle on antibiotic resistance than ophthalmologists practicing in the community, said Dr. Blomquist, because disease trends first become apparent in that “frontline” setting. Thus, he urged greater communication between ophthalmologists and local ER staff.
“You have to be aware of the organisms in your area and their susceptibility to the various antibiotics. You have to know the prevalence of drug-resistant strains so that you can cover them appropriately,” said Dr. Blomquist.
 |
|
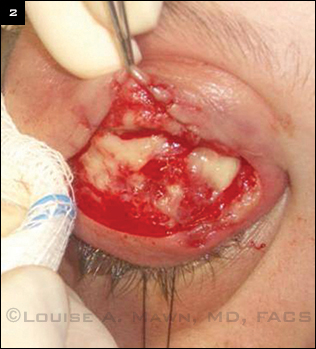
UNDER THE SURFACE. Intraoperative photograph shows areas of yellow purulence characteristic of S. aureus infection.
|
Orbital cellulitis. For empiric treatment of orbital cellulitis in MRSA-endemic areas, Dr. Blomquist recommends intravenous vancomycin and a broad-spectrum antibiotic. Drainage of focal abscesses is also an important part of the treatment regimen.
If you catch orbital cellulitis early and clear up the infection appropriately, there’s a great chance that the patient will have no sequelae, said Dr. Durairaj. “It’s the patients who only receive treatment much later in the course of the infection where we see catastrophic vision loss, an inability to move the eye, and other dire outcomes,” he said.
___________________________
1 Witherspoon SR, Blomquist PH. Ophthalmology. 2007;114(7):1420-1421.
2 Blomquist PH. Trans Am Ophthalmol Soc. 2006;104:322-345.
3 Kruger M et al. Retrospective review of ophthalmic MRSA infections from 2005 to 2009 at Parkland Memorial Hospital. Presented at: Association for Research in Vision and Ophthalmology Annual Meeting; May 2, 2011; Fort Lauderdale, Fla.
4 Mathias MT et al. Ophthalmology. 2012;119(6):1238-1243.
___________________________
Preston H. Blomquist, MD, is Dr. W. Maxwell Thomas Chair in Ophthalmology, professor and vice chair for education, and residency program director for the department of ophthalmology at University of Texas Southwestern Medical Center. Financial disclosure: None.
Vikram D. Durairaj, MD, is professor of ophthalmology and otolaryngology and chief of oculoplastic and orbital surgery at the University of Colorado Denver School of Medicine. Financial disclosure: None.
David G. Hwang, MD, is professor of ophthalmology, codirector of the cornea service, and director of the refractive surgery service at the University of California, San Francisco. Financial disclosure: None.