Download PDF
Patients with uveitis—whether intermediate, posterior, or panuveitis—can achieve similarly favorable results with either fluocinolone acetonide implants or systemic corticosteroids, often supplemented with immunosuppressive agents. These were the findings of a recent Multicenter Uveitis Steroid Treatment (MUST) trial, which identified factors linked to best-corrected visual acuity (BCVA) at baseline and 2 years later in 479 eyes from 23 clinical centers.1
“There’s a common perception that uveitis patients do badly,” said John H. Kempen, MD, lead author and professor of ophthalmology and epidemiology at the University of Pennsylvania. “But this study shows that even severe cases, on average, do well with the appropriate management.”
Predictive factors. Which patients had worse vision, and where did they end up? As expected, patients 50 and older had baseline BCVA that was worse than in younger patients. Patients with posterior uveitis also presented with significantly poorer vision than other categories of uveitis. However, both of these groups’ vision improved equally during the follow-up period of the study.
In fact, many patients with poor vision improved substantially. “Those with 20/50 vision or worse improved by 10 letters on average,” said Dr. Kempen. “Patients with near-normal vision improved modestly, but they had little room for improvement,” owing to a ceiling effect.
Inflammation control. Eyes presenting with more prolonged or severe inflammatory damage had much worse VA at baseline. However, these patients also did more poorly during the follow-up even when being treated aggressively according to the protocol, said Dr. Kempen. This observation made the researchers wonder whether earlier intervention might have improved their outcomes, he said. “We don’t have conclusive proof from this study, but there is a suggestion that early referral for state-of-the-art treatment might benefit these patients.”
It’s not a big surprise that control of inflammation is beneficial, but published research suggests that an important number of ophthalmologists compromise on this, said Dr. Kempen. “They may be worried about risks of using corticosteroids and immunosuppressive drugs. However, the systemic therapy arm of the MUST trial showed that systemic side effects were remarkably modest and similar to those of the implant.” The implant does produce local side effects, such as elevated intraocular pressure, but these typically can be managed well when they occur, he said, reinforcing the value of aggressive treatment.
Level of confidence. The study findings can provide fairly high levels of confidence for a variety of reasons, said Dr. Kempen. “We used gold standard methods for ascertaining visual acuity over time—a half-hour standardized refraction at every visit.” In addition, patients were followed using a common protocol that was strictly enforced across centers, and treatment regimens followed expert panel guidance.
Study limitations. The patients in the trial were drawn from tertiary centers, so their uveitis might have been more severe than that generally seen by comprehensive ophthalmologists. Further, although MUST was a randomized trial, the analysis reported in this paper was not the question directly addressed by randomization, making this report similar to an observational study. Confirmation in another study would be desirable, according to Dr. Kempen.
Hopeful results. “This paper shows that patients do really well if we move on to the immunologic or implant paradigm when it is justified,” said Dr. Kempen. This is particularly welcome news, given that uveitis can impact vision decades earlier than age-related diseases. “If we are not prepared to provide such treatment ourselves, we should send patients to someone who will.”
—Annie Stuart
___________________________
1 Kempen JH et al. Am J Ophthalmol. Published online Sept. 16, 2015. doi:10.1016/j.ajo.2015.09.017.
___________________________
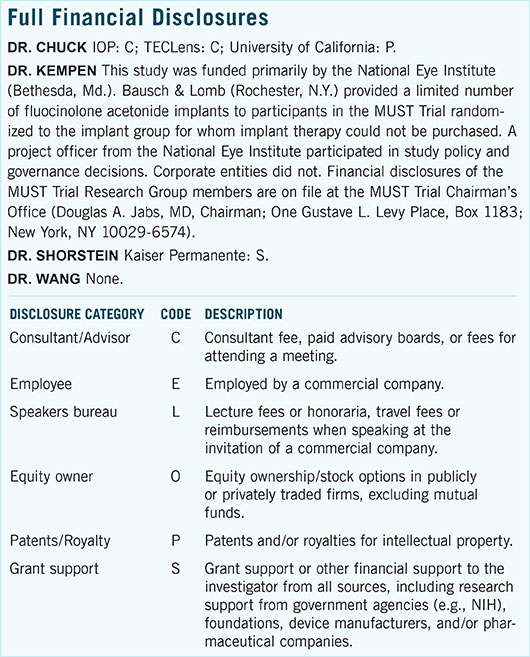
Relevant financial disclosures—Dr. Kempen: National Eye Institute: S; Bausch + Lomb: S.
For full disclosures and disclosure key, see below.
More from this month’s News in Review