NOTE: This article has been updated since print publication. In the original article, EyeNet incorrectly stated that herpesvirus is an RNA virus. It is a DNA virus. The article below removes the erroneous mention of RNA.
Download PDF
When Ebola virus survivor Ian Crozier, MD, was discharged from Emory University Hospital in October 2014, he had no detectable virus in his blood, and his visual acuity with eyeglasses was 20/15. But an occasional burning sensation, light sensitivity, and slight difficulty reading led him to consult Emory ophthalmologist Steven Yeh, MD, a month later—and thus began an unprecedented investigation of late-onset Ebola virus–associated uveitis in someone lucky enough to survive Ebola’s systemic effects.
Dr. Yeh and Jessica G. Shantha, MD, a senior ophthalmology resident at Emory who has since started her medical retina fellowship, were part of a multidisciplinary team that reported on Dr. Crozier’s case in The New England Journal of Medicine.1
The paper documented this previously reported,2,3 but largely uninvestigated and overlooked, late complication of Ebola infection. It also added some key information about ocular Ebola, including the discovery that the virus was not present in the conjunctiva or in tears—and that it can grow rapidly inside the eye. But many questions remain unanswered, Dr. Yeh and other uveitis subspecialists say.
What Caused the Inflammation?
“At a very fundamental level, much of this is not understood. Are the ocular manifestations due to increased replication of the virus, or is it the body’s reaction to the virus that’s causing the problem?” asked James P. Dunn Jr., MD, director of the uveitis unit at Wills Eye Hospital.
“The answer has enormous clinical implications. If the problem is the host immune response, which is in a sense overreacting, then you’re going to treat that with anti-inflammatories. If the problem is simply the virus causing damage, you’re going to focus on treatment for the virus itself,” Dr. Dunn said. Dr. Yeh noted, “The laboratory findings suggest that rapid viral replication is having a cytopathic effect and leading to the inflammation.”
It also is unclear how and when the virus entered the eye, and why severe ocular symptoms took more than 3 months to develop after the initial viral infection, said Quan D. Nguyen, MD, at the University of Nebraska’s Truhlsen Eye Institute, in Omaha. Dr. Yeh said that the patient’s severe uveitis began 100 days after his initial Ebola diagnosis and 2 months after the viremia had abated.
“I think that the virus was probably already there in the eye, dormant. But it will take more research for us to know if that is the case; and, if so, what activated the virus to begin replicating,” Dr. Nguyen said.
A second uveitis case, for comparison? Dr. Nguyen said he personally knows of a second American Ebola survivor who developed uveitis about 10 days after being cleared of viremia and released from hospitalization in the biocontainment unit at the University of Nebraska Medical Center in Omaha.
“While he was here, he did not have any apparent ocular inflammation,” Dr. Nguyen said. “About 10 days or so after he returned home, he presented with acute uveitis. I know this because his ophthalmologist called me and asked if we had seen any uveitis when the patient was here.”
A report on the case has not been published, he said.
Dr. Crozier’s Clinical Course
The New England Journal of Medicine published details of Dr. Crozier’s case.1
Initial findings. When first examined by Dr. Yeh and Dr. Shantha in November, Dr. Crozier had bilateral asymptomatic, pigmented chorioretinal lesions in the retinal periphery with atrophic hypopigmented halos around them. “The diagnosis was asymptomatic posterior uveitis, which looked like chorioretinitis. The findings were similar to what you see with a West Nile virus infection,” Dr. Yeh said. The patient’s bilateral visual acuity with eyeglasses was 20/15, IOP was 10 mm Hg in the left eye and 9 mm Hg in the right, and the vitreous was quiet.
Day 1: high IOP, inflammation. One month after his first visit, Dr. Crozier returned, complaining of eye pain and redness, halos, blurred vision, and photophobia in the left eye. In that eye, his IOP was 44 mm Hg, VA had declined to 20/20, and 2+ stromal haze and 2+ vitreous haze were present. The diagnoses were unilateral anterior uveitis and ocular hypertension. “His pressure was extremely high, and he was in intense pain. That’s how we ended up putting him on a number of topical and oral medications pretty quickly,” Dr. Yeh said. These included oral acetazolamide and topical prednisolone, brimonidine, dorzolamide, and timolol.
Day 4: low IOP. Despite increased dosing frequency of the prednisolone and the addition of topical atropine over the ensuing 48 hours, anterior chamber inflammation increased. IOP in the affected eye was 6 mm Hg, and VA decreased to 20/25.
Day 5: anterior chamber paracentesis. After obtaining a conjunctival swab and taking tear film samples, Dr. Yeh and Dr. Shantha withdrew 170 μL of aqueous from the anterior chamber to have it tested for Ebola virus. (See “Extraordinary Measures: The Paracentesis” below.) This confirmed a high concentration of Ebola in the anterior chamber and the absence of virus in the conjunctiva and tears.
Days 6 and 7: acuity falls. Although the IOP had returned to 15 mm Hg in the left eye by day 6, Dr. Crozier’s VA continued to fall to 20/60 on the sixth day and 20/150 on the seventh. Vitritis was noted. The hypotensive drugs were discontinued, and oral prednisone was added to the medication regimen.
Days 10-14: hypotony and the VA nadir. The pain level was improving, the scleritis resolved, and anterior chamber inflammation decreased; but vitritis and VA worsened. On day 10, the patient received a periocular injection of triamcinolone, and he began 21 days of oral antiviral therapy with the investigational drug favipiravir (T-705; MediVector). Topical difluprednate was prescribed, plus a 10-week tapering course of oral prednisone.
Meanwhile, VA in the affected eye dropped to 20/800 (hand motions) on the tenth day and fluctuated between that and 20/400 over the next 4 days. There was choroidal edema as well as edema around the optic nerve head. IOP plunged to 4 mm Hg on day 10, then as low as 1 mm Hg on days 11 to 14.
Dr. Dunn suggested that the extreme hypotony might have occurred because the virus, which in other organs replicates in epithelial cells,4 was infiltrating the ciliary body epithelial cells that secrete aqueous.
Slow improvement. Dr. Crozier’s condition continued to worsen, and periocular triamcinolone was administered. Eventually, the inflammation began subsiding, and Dr. Crozier slowly began to recover his vision, Dr. Yeh said. Three months after the uveitis was diagnosed, VA in the affected eye measured 20/15, he said.
Extraordinary Measures: The Paracentesis
As Dr. Crozier’s uveitis quickly worsened, Dr. Yeh said that he, Dr. Shantha, and the team suspected that the underlying cause was intraocular Ebola or another virus, such as cytomegalovirus, herpes, or varicella-zoster. However, because medications that work against these other viruses are ineffective against Ebola, it was essential to know which microbe was the culprit. So they donned personal protective equipment, using safety precautions that they had discussed with the Serious Communicable Diseases Unit at Emory University Hospital, and performed paracentesis of the anterior chamber—thereby putting themselves at possible risk of Ebola exposure.
A subsequent reverse transcription polymerase chain reaction assay confirmed that their caution had been warranted: The anterior chamber was teeming with Ebola. “The viral concentration in the aqueous was higher than it was in his blood when he was critically ill,” Dr. Yeh said.
Despite having observed all possible protective measures while collecting the aqueous, after this procedure Dr. Yeh slept in a spare bedroom and did not hold his infant son for 21 days, Ebola’s incubation period. Both Dr. Yeh and Dr. Shantha also underwent 21-day temperature and symptom monitoring during this period.
“It was pretty intense, when you think of how much live virus was in that sample,” Dr. Yeh said.
|
Understanding Uveitis Better
In addition to highlighting how little is known about the long-term impact of Ebola in survivors, Dr. Crozier’s case eventually might illuminate some of the mechanisms of ocular inflammation, viral infection, and uveitis, Dr. Dunn said. He gave 2 examples:
Idiopathic uveitis. Perhaps viral infections can explain these cases, he said. “A significant number of patients with uveitis have no identifiable cause. So it is interesting to theorize how many patients who are exposed to much less lethal viruses might go on to develop uveitis, no cause of which is ever found, and then get better spontaneously or with steroid therapy.”
Early scarring. The pigmented chorioretinal scars with atrophic halos that Dr. Crozier had in the earliest phase of his uveitis are “not uncommon” to see during normal ophthalmic exams, Dr. Dunn said. “Many of these scars are attributed to toxoplasmosis. But my suspicion is that some of them are related to other types of viruses, particularly when they’re bilateral.”
Unanswered Questions
Dr. Yeh, Dr. Shantha, Dr. Crozier, and Brent Hayek, MD, an Emory oculoplastic surgeon, traveled to Liberia in April to evaluate approximately 100 Ebola survivors with the constellation of medical problems, including uveitis, that is sometimes referred to as “post-Ebola syndrome.”
A number of questions remain regarding why uveitis develops in some patients. Chief among these questions is where in the eye the Ebola virus was hiding for 100 days, and what triggered its reactivation. In lab animals and cell lines, hints are emerging that the trigger might come from the patient’s own dysregulated immune system, Dr. Yeh said. “The eye is a very well-regulated organ, and these regulatory mechanisms must be allowing the virus to persist quietly in the eye until replication is somehow triggered,” he said. “This might explain why Ebola outbreaks appear to occur in seemingly random patterns in different parts of the world at different times. Maybe it’s not random at all but actually reflects nature’s way of waking up a dormant virus.”
Other questions include:
How typical was Dr. Crozier’s clinical course, which began with asymptomatic posterior uveitis, followed by anterior uveitis and then severe panuveitis? “We don’t know if that’s the typical course, or if other patients follow a different progression,” Dr. Dunn pointed out.
Which therapies, if any, are responsible for Dr. Crozier’s visual recovery? Did the antiviral favipiravir help or hurt? “You can’t look at this and say that the favipiravir was the magic bullet,” Dr. Dunn said. “We know that some antivirals such as cidofovir can actually cause uveitis as well as hypotony. Is it possible that the favipiravir caused his hypotony? Probably not, but did it make it worse?”
Dr. Yeh added that it is unknown whether treatment with favipiravir clears the virus completely from the eye. However, some viruses, such as herpesvirus, are known to persist in dormant form, and they are capable of causing disease under the right conditions, he said.
Laboratory studies indicate that favipiravir prevents viral replication by inhibiting synthesis of RNA genomes and messenger RNAs and that it might be effective against a variety of RNA viruses. (The drug is in phase 3 trials in the United States for treating influenza; a fast-track federally funded Ebola trial is being planned.)
How does genetic variability affect susceptibility? The sparse literature on Ebola survivors indicates that up to 40% develop late uveitis.2 Genetics might help explain why the disease does not occur in all survivors, Dr. Nguyen said. “Clearly, some patients might be born with some level of immune dysregulation that remains quiet without any disease manifestations until there is an external factor, like in this case a viral infection,” he said. “So you would have perhaps an infectious etiology that tips the balance of the immune system, causing a dysregulation that leads to overly active inflammatory processes.”
2 Take-Home Messages
1. Take precautions with post-Ebola patients. The Academy responded to Dr. Crozier’s case by issuing a statement that advises members to take special precautions5 when treating patients who are or have been infected with Ebola. “The newest findings that indicate uveitis may be associated with active virus within the eye highlight the vital importance of such safety measures for ophthalmic health care professionals when performing invasive procedures such as intraocular injections or surgery for cataracts or glaucoma on patients who have been infected with the Ebola virus,” the Academy’s statement says.
2. Recognize aggressive uveitis early. Dr. Nguyen advises ophthalmologists on the front lines of patient care to act quickly and emphatically to suppress the inflammation when a patient presents with uveitis that might be associated with a virus, especially Ebola.
“Sometimes, if it’s a mild virus, it will affect only the anterior portion of the eye,” Dr. Nguyen said. He added that the lesson physicians should learn is that if uveitis occurs in the setting of very severe viremia, they should anticipate that it will not be a relatively benign anterior uveitis—“but an aggressive panuveitis that therefore requires very aggressive treatment, with a multimodal approach of delivering the medication to control the inflammation.”
___________________________
1 Varkey JB et al. N Engl J Med. 2015;372(25):2423-2427.
2 Bwaka MA et al. J Infect Dis. 1999;179(suppl 1):S1-S7.
3 Mupupa KD et al. J Infect Dis. 1999;179(suppl 1):S13-S14.
4 Kindrachuk J et al. J Virol. 2014;88(17):9877-9892.
5 www.aao.org/clinical-statement/ebola-virus-disease--what-ophthalmologists-need-to.
___________________________
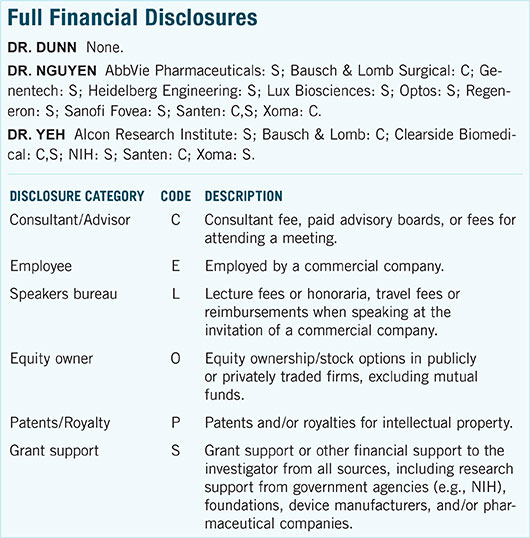
Dr. Dunn is professor of ophthalmology at Sidney Kimmel Medical College of Thomas Jefferson University, Philadelphia, and director of the uveitis unit of the retina division at Wills Eye Hospital. Relevant financial disclosures: None.
Dr. Nguyen is McGaw Professor of Ophthalmology, department chairman, and inaugural director of Truhlsen Eye Institute, at the University of Nebraska Medical Center, in Omaha. Relevant financial disclosures: AbbVie Pharmaceuticals: S; Bausch & Lomb Surgical: C; Genentech: S; Heidelberg Engineering: S; Lux Biosciences: S; Optos: S; Regeneron: S; Sanofi Fovea: S; Santen: C,S; Xoma: C.
Dr. Yeh is associate professor of ophthalmology, and director of the section of uveitis and vasculitis, section of vitreoretinal surgery & diseases, at Emory Eye Center, Emory University, Atlanta. Relevant financial disclosures: None.
For full disclosures and the disclosure key, see below.
___________________________
MORE ONLINE. View the ARVO 2015 Closing Keynote “Ebola and the Eye: A Story of Discovery and Uncertainty.”