Download PDF
Recently revised diagnostic criteria for neuromyelitis optica (NMO), now called neuromyelitis optica spectrum disorder (NMOSD), should make it easier for ophthalmologists to identify optic neuritis caused by this inflammatory disease of the central nervous system.1 The spectrum disorder can affect the optic nerves, brainstem, spinal cord, and brain.
“Eye M.D.s are in an important position to recognize this disease [NMOSD] at presentation,” said Mayo Clinic neurologist Dean M. Wingerchuk, MD, FRCPC, who cochaired an international panel that developed the criteria.
The new criteria are expected to facilitate earlier and more accurate diagnosis by helping doctors identify individuals who might otherwise have been diagnosed with idiopathic transverse myelitis, idiopathic optic neuritis, or atypical multiple sclerosis, said Dr. Wingerchuk, professor of neurology, and chair of the Division of Multiple Sclerosis and Autoimmune Neurology, at the Mayo Clinic in Scottsdale, Ariz.
The criteria. The 2015 diagnostic criteria outline a stratified diagnosis based on the presence or absence of serum aquaporin-4 immunoglobulin G antibodies (AQP4-IgG), which are highly specific for NMOSD. Most—though not all—patients with NMO have detectable serum antibodies that target AQP4-IgG. The new criteria address both sets of patients, and they establish more stringent diagnostic criteria for cases in which the antibodies are not detectable or for which the diagnostic blood test is not available. (Diagnostic criteria for both groups are presented in the Web Extra below.)
“Now a diagnosis of NMOSD with AQP4-IgG can be confidently made, even if a patient has experienced neither optic neuritis nor transverse myelitis,” said Dr. Wingerchuk.
These new diagnostic criteria should help to increase awareness of NMOSD and allow diagnosis after a single clinical event, if a patient is AQP4-IgG seropositive. For those who are not seropositive, the new criteria also explicitly describe the clinical and MRI features of the disease. Those features have been expanded to include abnormalities of the brainstem, diencephalon, and brain.
Challenging cases. “Ophthalmologists must be aware of NMOSD when seeing patients with optic neuritis, whether it is a first, apparently isolated, event or occurring in the context of other neurological symptoms,” Dr. Wingerchuk said. “More severe events of optic neuritis—those with poor recovery, bilateral optic nerve or chiasmatic involvement, and primary involvement of the posterior aspect of the optic nerve—are clues that the optic neuritis event could be caused by NMOSD.” When confronted with a challenging diagnosis, he advised ophthalmologists to consider further diagnostic evaluation such as brain and orbital MRI and serum AQP4-IgG testing.
Treat early. He added that, if warranted, the ophthalmologist should consider referral to a center with NMOSD experience because seropositive patients are candidates for immediate long-term immunosuppressive therapy to prevent attacks. “The point is to facilitate early treatment because AQP4-IgG seropositive patients who have had even one attack are at high risk for relapse and disability. Long-term immunotherapy is indicated,” he said.
Dr. Wingerchuk expressed the hope that new scientific advances will make it easier to diagnose patients with NMOSD who don’t have detectable AQP4IgG antibodies and, thus, are more diagnostically difficult than seropositive patients.
For now, he said to be aware that NMOSD encompasses more than optic neuritis and transverse myelitis. “Ophthalmologists should consider the [NMOSD] diagnosis and diagnostic testing when faced with central nervous system inflammatory disease of wider spectrum, including the brain.”
—Miriam Karmel
___________________________
1 Wingerchuk DM et al. Neurology. 2015;85(2):177-189.
___________________________
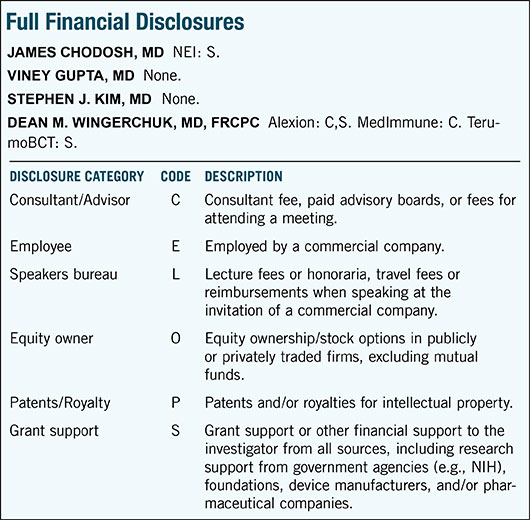
Relevant financial disclosures—Dr. Wingerchuk: Alexion: C,S; MedImmune: C; TerumoBCT: S. All are companies that do research on NMOSD treatments.
For full disclosures and disclosure key, see below.
More from this month’s News in Review