By Linda Roach, Contributing Writer, interviewing David P. Crabb, PhD, Stuart Gardiner, PhD, Felipe A. Medeiros, MD, PhD, and Joshua D. Stein, MD, MS
Download PDF
Some novel ideas about improving visual field (VF) testing are emerging in the glaucoma research community, and even though more work is needed, they are inspiring new ways of thinking.
Researchers are trying to make VF tests better predictors of disease progression, by applying sophisticated statistical and system modeling techniques to thousands of test results collected in large clinical trials1 and by using simple linear regression plots to demonstrate that clustering tests would improve detection.2,3
The Challenge: Variable Data
Retinal sensitivity measurements taken with standard automated perimetry (SAP) remain a criterion for clinical decision-making in glaucoma, even though mean deviation (MD) and pattern standard deviation (PSD) data from SAP tests are highly variable, said Stuart Gardiner, PhD, at Devers Eye Institute in Portland, Ore.
“The more damage you have, the more variable the data get. We’re learning more about that variability, but we just haven’t been able to get rid of it,” Dr. Gardiner said. “Typically in America, there is a 24-2 test pattern, which samples 54 locations, 4 or 5 times each. This isn’t enough stimulus presentations to test any one of the locations accurately. But patients find the test unpleasant,4 so increasing the duration of the test is not practical.”
The variability remains problematic even when equipment makers try to assist clinicians by combining the locations into a single unified index, such as the Visual Field Index (VFI), he said. Dr. Gardiner said his ongoing research has found that the VFI, which rates fields on a scale of 0 to 100, detects reduced sensitivity to stimuli later in disease progression than the MD does.
“In the majority of eyes, VFI cannot detect early damage. You can have quite a lot of loss, and it will still say you’re at 100%,” Dr. Gardiner said. “At the other end of the scale, when damage is severe, the numbers jump around quite a lot.5 And the VFI considers not being able to respond to any stimuli, anywhere in the field, as 0% vision. It will say that you have no vision at all—when that’s not true.”
 |
|
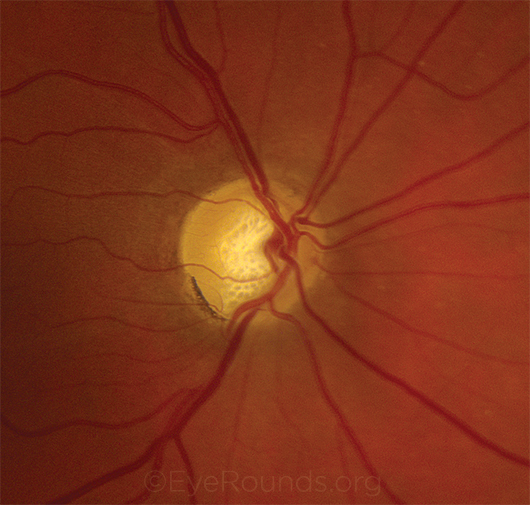
TAILORING TREATMENT. Ideally, VF models that predict rapid progression will allow clinicians to develop targeted treatment plans. Shown here: optic nerve damage from severe POAG.
|
A Personalized Solution?
To bypass such limitations, a multidisciplinary team at the University of Michigan developed a Kalman filter– based algorithm that incorporates information on a glaucoma patient’s past and current intraocular pressure measurements and VF test results to generate a personalized prediction of the stability or progression of that individual’s disease,1 said Joshua D. Stein, MD, MS, at the University of Michigan.
If this model is further validated, the algorithm’s forecasts could give clinicians a more reliable, objective tool to individualize each patient’s VF testing schedule and, consequently, lead to more timely detection of disease progression and aid clinicians with treatment decisions, Dr. Stein said.
Introduced in the 1960s, the Kalman filter was originally developed to strip unwanted statistical “noise” from dynamic streams of data, notably those necessary for complex navigational tasks (including the Apollo 11 moon landing).6 More recently, medical researchers have explored the technique to help physicians optimally monitor disease markers in chronic conditions such as diabetes and prostate cancer.7
Testing the model in POAG. Dr. Stein and his engineering colleagues used existing data from 2 large-scale glaucoma treatment trials8,9 to build a model of disease progression in patients with moderate to severe primary open-angle glaucoma (POAG).1
“Unlike most tools that compare patients to normative databases, our model learns the unique glaucoma progression dynamics for each patient and uses that information, along with the progression dynamics for patients from the trials, to predict the trajectory of each patient’s glaucoma into the future,” Dr. Stein said. “Each time the patient takes a new test, the algorithm updates its predictions.” The group calls their algorithm ADVISE-GM (for “Advanced Diagnostics, Visualization and IOP Systems Engineering—for Glaucoma Management”).
Faster diagnosis? If the algorithm had been available in the trials on which it was based, it would have improved the overall efficiency of identifying progression by 29%, compared with fixed yearly testing schedules, Dr. Stein and his colleagues found. This also would have reduced the time to identification of progression by 57% compared with a fixed annual testing schedule.1
Dr. Gardiner said that tools such as ADVISE-GM can provide earlier detection of change in a “typical” glaucoma patient. “But this comes at the cost of potentially missing unusual patterns of change and nonglaucomatous changes” to the VF, he added. “Clinically, these tools can assist, but should not replace, careful consideration of all aspects of the individual patient’s test results.”
Algorithm to be expanded. Dr. Stein said he and collaborator Mariel Lavieri, PhD, have received National Eye Institute funding to incorporate optical coherence tomography (OCT) values into the algorithm and to validate it in patients with ocular hypertension. “Then the next step will be to test the tool prospectively on patients in a real-world setting,” he said.
Internet access planned. Meanwhile, the researchers plan to modify the tool so that it can be posted online for eye care providers to try out by plugging their patients’ VF data into a form, Dr. Stein said. They hope to have this available as soon as early 2017.
An online calculator is an important way for the Kalman filter algorithm or any other heavily mathematical tool to have an impact on patient care, said David P. Crabb, PhD, at the City University of London. “It doesn’t matter whether I think I have a good method. Clinicians are not going to use these methods unless they have software available to use them,” he said.
Rethinking Test Timing
How often should a glaucoma patient undergo VF testing? In 2012, Dr. Crabb and David F. Garway-Heath, MD, who have collaborated on many studies of testing protocols, reported on computer simulations that challenged conventional wisdom about how often to test VF in newly diagnosed patients.2
Their conclusions: More testing is better, but only if done in clusters of 3 tests. Furthermore, they found, performing a single VF test per year (a common practice) is insufficient. “Doing the odd VF test in every patient once or less per year is probably as bad as not doing it at all,” they wrote.
Support from simulations. If VF tests on 200 newly diagnosed patients were spaced at 4-month intervals for 2 years, totaling 7, almost as many patients would be falsely identified with rapid progression as would be correctly identified (12 versus 16, respectively), computer simulations showed.2
But if the tests were clustered into 3 tests at baseline and 3 at the end of 2 years, 19 out of 20 rapidly progressing patients in the group would be correctly identified, and there would be no false positives. Below 4 or 5 tests in a 2-year period, nearly half of the rapid progressors would be missed—and a single VF test per year would be even worse, the study found.
“Visual field testing is all about separating the signal from the background noise,” Dr. Crabb explained. “And if you increase the number of tests by doing them in a cluster, then you improve your chances of detecting that signal against the background noise.”
Support from UKGTS. Armed with these conclusions, Drs. Crabb and Garway-Heath incorporated clustering of visual field tests at baseline, 18 months, and 24 months into the UK Glaucoma Treatment Study (UKGTS).3
This triple-masked trial randomized 516 newly diagnosed POAG patients to latanoprost or placebo eye drops. The test clustering enabled the researchers to detect statistically significant differences in VFs between treated and untreated patients after the previously unheard-of observation period of 12 months. “The UKGTS has the shortest observation period of any glaucoma trial with a vision function outcome, with a difference between treatment groups evident at only 12 months, as well as at the planned 24-month analysis time point,” the researchers said.
Potential Clinical Tool
Dr. Crabb and his colleagues believe that the UKGTS demonstrated that clinicians could improve the utility of VFs by adopting the following strategy: performing an initial cluster of VF tests (over a period of 1-2 weeks), followed by another test cluster about 2 years later. “This would be one of the simpler things you could do to find rapid progressors. And then maybe those would be the patients who would be the candidates for further testing, such as OCT,” Dr. Crabb said.
This change in practice would not require ophthalmologists to perform complicated mathematics, he pointed out. “We used a linear regression technique, plotting the visual field measurements to try to fit some kind of trend line to them,” he said. “Then we did the same thing with the next test cluster and compared the slopes of the trend lines to look for a change indicating a loss in visual function.”
Need for further validation. However, Felipe A. Medeiros, MD, PhD, said that further validation is necessary before a 2-year wait between VF tests can be generally recommended. “The simulation results are certainly very interesting and promising, but there are additional issues that need to be considered,” said Dr. Medeiros, at the University of California in San Diego.
“For example, doing clusters of tests once every couple of years may lead to a false sense of confidence that the disease is well controlled, which could, in some cases, lead to loss of follow-up or decreased compliance by patients,” he said. “In addition, the simulations are all based on the assumption that VF loss will occur linearly over time, an assumption for which there is really not good evidence.”
He concluded, “The approach could be valuable to many patients and result in better allocation of resources. We just need to better define which patients are likely to benefit the most.”
___________________________
1 Schell GJ et al. Ophthalmology. 2014;121(8):1539-1546.
2 Crabb DP, Garway-Heath DF. Invest Ophthalmol Vis Sci. 2012;53(6):2770-2776.
3 Garway-Heath DF et al. Lancet. 2015;385(9975):1295-1304.
4 Gardiner SK, Demirel S. Ophthalmology. 2008;115(12):2127-2131.
5 Rao HL et al. Invest Ophthalmol Vis Sci. 2013;54(1):307-312.
6 Cipra B. SIAM News. 1993;26(5). Reprinted online at www.cs.unc.edu/~welch/kalman/siam_cipra.html. Accessed Sept. 6, 2016.
7 Kuure-Kinsey M et al. Conf Proc IEEE Eng Med Biol Soc. 2006;1:63-66.
8 Musch DC et al; CIGTS Study Investigators. Ophthalmology. 2009;116(2):200-207.
9 AGIS Investigators. Am J Ophthalmol. 2002;134(4):499-512.
___________________________
Dr. Crabb is professor of statistics and vision research at the City University of London, England. Relevant financial disclosures: Allergan: C.
Dr. Gardiner is associate scientist at Devers Eye Institute in Portland, Ore. Relevant financial disclosures: Haag-Streit: C; NEI: S.
Dr. Medeiros is the Ben and Wanda Hildyard Chair for Diseases of the Eye, professor of clinical ophthalmology, medical director and director of Visual Function Research, and fellowship program director at the Hamilton Glaucoma Center of the Shiley Eye Institute at the University of California, San Diego. Relevant financial disclosures: Alcon: S; Allergan: C,S; Bausch + Lomb: S; Carl Zeiss Meditec: C,S,P; Heidelberg Engineering: S; NEI: S; Novartis: C; Merck: S; Reichert: S; Sensimed: S; Topcon: S.
Dr. Stein is associate professor of ophthalmology and visual sciences, associate professor of health management and policy, and director of the Center for Eye Policy and Innovation at the University of Michigan in Ann Arbor. Relevant financial disclosures: None.
See the disclosure key at www.aao.org/eyenet/disclosures.