This article is from May 2005 and may contain outdated information.
For nearly half a century, Goldmann applanation tonometry has been the reigning standard for routine measurement of IOP. Despite its inherent shortcomings, nothing has come along to take its place. Now, several devices—designed to measure IOP independent of confounding corneal properties—are poised to challenge Goldmann’s 50-year run. It’s too early to say whether any one of these alternatives will become the new standard. But glaucoma specialists familiar with them agree that if studies pan out, ophthalmologists will have a tool that better measures true IOP.
“Another ‘gold standard’ is what we’re trying to develop,” said Brian A. Francis, MD, assistant professor of ophthalmology, University of Southern California, who is testing the devices in three investigations. “I think we’re near that,” he said, adding that these promising technologies still need to undergo big trials.
The limitations. From the start, Hans Goldmann, MD, acknowledged the limitations of his invention, which was based on an invalid assumption that the corneas of all eyes varied only slightly. The accuracy of Goldmann applanation tonometry depends on several factors, including corneal shape (radius and astigmatism), elasticity, rigidity and, most notably, corneal thickness. Pressure readings tend to be overestimated in thick and more rigid corneas, and underestimated in thinner corneas, leading to misdiagnosis of glaucoma.
Still, Goldmann is the device that has prevailed. “We didn’t have anything better,” said Robert L. Stamper, MD, professor of ophthalmology at the University of California, San Francisco, who also has studied the new devices. “For the most part, [Goldmann] worked pretty well.” Besides, he added, “Nobody thought it was a problem. We were patting ourselves on the backs, saying we are so much better off than with the old [devices]. . . . We assumed we’d reached nirvana, and people turned their attention [to other matters].”
More recent findings. In 2004, a study by Leon W. Herndon, MD, associate professor of ophthalmology at Duke University, found that corneas varied much more widely in corneal thickness than Dr. Goldmann had assumed.1 And the Ocular Hypertension Treatment Study (OHTS) found that thin corneas are a risk factor for conversion from ocular hypertension to open-angle glaucoma. Another study suggested that they were a risk factor for the progression of normal-tension glaucoma. “OHTS reignited interest in the issue of corneal thickness and IOP measurement,” Dr. Stamper said. (Additionally, it has been recognized that the effects of LASIK surgery render accurate IOP measurement by standard applanation tonometry difficult or impossible.)
Since OHTS, doctors are advised to measure corneal thickness along with IOP. But the existing nomograms that adjust for corneal thickness are considered unsatisfactory. Hence the search for a device that measures pressure independent of corneal variables. Glaucoma specialists most often mention two devices: the PASCAL dynamic contour tonometer and the Reichert Ocular Response Analyzer.
 |
|
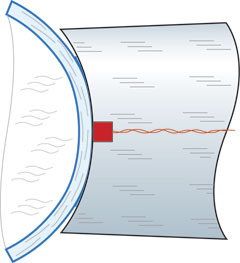
PASCAL PROBE. The PASCAL’s probe rests on the relaxed cornea with a constant force of one gram. Its piezoelectric sensor measures IOP 100 times per second.
|
Dynamic Contour Tonometer
The PASCAL dynamic contour tonometer (DCT) is a slit lamp–mounted device designed to measure IOP independent of corneal rigidity or thickness. It received FDA clearance in November 2003 and was commercially launched
in August 2004.
How it works. PASCAL has a concave tonometer tip that matches corneal curvature and measures pressure directly by means of a miniaturized, built-in sensor. When it touches the cornea it allows the cornea to assume its natural shape when pressure on both sides is equal and distortion of the cornea is minimal. DCT is different from applanation tonometry. “It’s a new principle, a new concept,” said Dr. Stamper, who has conducted two DCT studies.
Study results. In Dr. Stamper’s studies (performed on eye bank eyes rather than in vivo), the Pascal was more accurate than other tonometers. It provided the most accurate IOP readings within ± 0.7 mmHg, whereas Goldmann readings were consistently below true IOP by an average of 4 mmHg. Pneumatonometry also furnished values lower than true IOP, with the error increasing markedly at higher pressures. Dr. Stamper concluded that the DCT “appears to be a promising new technology that is highly accurate and easy to use, and functions independently of corneal thickness and edema.”
Healthy eyes. One study of 228 healthy eyes with corneal thickness ranging from 439 to 642 micrometers, found excellent concordance of DCT measurements compared with those obtained by Goldmann applanation tonometry.2 What’s more, DCT readings showed lower observer variability.
LASIK eyes. In another study of 118 LASIK eyes in young, healthy patients, DCT proved to be better suited to monitor IOP than either Goldmann applanation tonometry or noncontact air puff tonometry.3
Current studies. Currently, the Los Angeles Latino Eye Study has enrolled more than 6,000 participants in a study that is trying to correlate Goldmann applanation tonometry and Pascal with regard to corneal thickness.
Another investigation is being conducted by Joel S. Schuman, MD, professor and chairman of ophthalmology at the University of Pittsburgh. He is looking at four different tonometers (applanation, pneumatonometry, TonoPen and dynamic contour tonometry) with regard to the effect on IOP of corneal thickness and curvature. The pressures are compared with intraoperative manometric readings. “We don’t really know all of the factors that affect IOP measurement with applanation tonometry,” Dr. Schuman said. “We know corneal thickness plays a role, but that there are other issues as well. Dynamic contour tonometry may address those factors. We just don’t know.”
The DCT has a couple of drawbacks: it’s more time consuming than Goldmann, and it doesn’t seem as useful in diseased corneas or after corneal transplant. Still, Dr. Schuman calls the DCT very promising. “It tends to read a little higher in general than applanation tonometry in people with thin or average thickness corneas. I’m very excited about it. The early data look good. The study isn’t complete. I can’t say with conviction exactly how much the DCT will help us to overcome these confounding [factors].”
Ocular Response Analyzer
The Ocular Response Analyzer is similar to Reichert’s current generation noncontact tonometer and provides a Goldmann-equivalent IOP reading. It analyzes the signal obtained from the corneal response to provide a new metric for measuring the biomechanical properties of the corneal tissue.
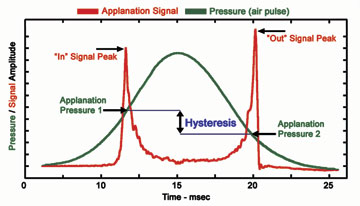
How it works. The Ocular Response Analyzer produces a rapid air impulse to apply force to the cornea, and uses an electro-optical system to monitor the deformation. The device records two applanation events: the first, while the cornea is moving inward; the other as it returns. The difference between the “in” and “out” pressure values is known as corneal hysteresis, which is a measure of viscoelastic damping, or the ability of the tissue to absorb and dissipate energy.
Study results. In a study released by Reichert, 32 eyes were measured at three different pressure levels, using both a Goldmann tonometer and an Ocular Response Analyzer. Initial IOP measurements were made on the eyes in a normal state followed by two artificially elevated pressure levels. The data show that hysteresis remains constant for the same set of corneas over a range of pressures, showing that hysteresis is independent of pressure in normal eyes.
The company speculates that it may be able to use corneal hysteresis alone or in combination with central corneal thickness measurements to develop an algorithm for more accurate IOP measurements. Studies are in progress.
Soft corneas. Reichert studies also have shown that subjects with “soft” corneas, or those exhibiting low corneal hysteresis, are probable candidates for a variety of ocular diseases and complications. The company says the device may be used to help identify and classify conditions such as corneal ectasia and Fuchs’ dystrophy. And it may be clinically useful in refractive surgery.
About 25 sites around the world are using the Ocular Response Analyzer. The device has been approved by the FDA and may become commercially available by late August.
 |
|
HOW ONE NEW DEVICE WORKS. The Reichert Ocular Response Analyzer measures the pressure values at applanation as the cornea is moving in and as it is moving out. The difference in values equals corneal hysteresis, which is a measure of viscoelastic damping.
|
Not Quite Ready for Prime Time
For now, the experts agree that more prospective studies are needed before any device replaces Goldmann.
Dr. Stamper continues to measure pressure the time-honored way, while also measuring corneal thickness on every patient. He tries to check pressures with the DCT, especially in patients with very thin or thick corneas. The DCT “provides another piece of information to confirm my prejudices,” he said. “It may help me feel a little better, if somebody has 25 [mmHg] and a thick cornea. Then I measure it with a Pascal and it’s 19. I’m a little more comfortable telling the patient to come back.”
High cost. While he believes the DCT is a useful adjunct, Dr. Stamper is not insensitive to cost. “There’s a practical issue here. It’s a moderately large investment.” (The base price is $5,655.)
Richard A. Cohn, MD, a glaucoma specialist in Winter Park, Fla., agrees. “Everything I’ve read about it [DCT] shows that it is rather accurate. It does take corneal thickness out of the equation, which is nice. But the problem with it is the expense to the general practitioner.”
Dr. Cohn said that he’s comfortable measuring IOP with the Goldmann, but he takes corneal thickness into account. As for the claim that there are no good nomograms to make that conversion, he said, “I’m not so sure about that. We’re looking for trends.”
He acknowledged, however, that the DCT would be useful on patients with really thick or thin corneas. “I just don’t think there’s going to be an overwhelming trend for everyone to throw away their Goldmann tonometers.”
Still, “it makes sense to have one [a DCT] so you can confirm your suspicions,” said Dr. Stamper. “The next few years will tell us whether it really will make a difference in our management of glaucoma.”
Practical measures. In the meantime, Dr. Stamper recommends that physicians perform pachymetry on every glaucoma suspect and glaucoma patient. “And they should at least understand the relationship between Goldmann tonometry and corneal thickness. Those who are concerned about knowing absolutely what the IOP is should give some thought to have at least one of these units.”
Dr. Schuman still uses applanation tonometry clinically, and he uses a pneumatonometer in patients whomay have confounding conditions, such as obesity or scarred corneas, or in patients who hold their breath. |While he finds the DCT promising, he’s reserving judgment until studies, such as his, are complete. “Until then, Goldmann remains the standard of care.” Dr. Francis concurs. “Goldmann is still the standard, but keep in mind adjustment factors for corneal thickness.”
______________________________
1 Herndon, L. W. et al. Arch Ophthalmol 2004;122:17–21.
2 Kaufmann, C. et al. Invest Ophthalmol Vis Sci 2004;45:3118–3121.
3 Siganos, D. et al. J Cataract Refract Surg 2004;30(4):746–751.
______________________________
None of the doctors has a financial interest in the technologies. Drs. Francis and Stamper have received instruments and some research funding from the companies manufacturing the devices. Pascal has provided Dr. Schuman with research loans of devices for the studies.