By Lori Baker-Schena, MBA, EdD, Contributing Writer, interviewing Mary Louise Z. Collins, MD, Joseph L. Demer, MD, PhD, and Amy K. Hutchinson, MD
Download PDF
Joseph L. Demer, MD, PhD, at the Stein Eye Institute in Los Angeles, can wiggle his ears. While this particular talent may not be relevant to most ophthalmology practices, its value is incalculable when he needs to examine a young nonverbal patient.
Indeed, these assessments demand unusual levels of patience, creativity, and ingenuity from the clinician. Ophthalmologists should never assume that nonverbal patients cannot see simply because they cannot respond to routine visual testing, said Amy K. Hutchinson, MD, at Emory Eye Center in Atlanta. “Instead, we must look for creative ways to examine these patients.”
Growing Patient Population
The need for clinicians who are skilled in the art of the nonverbal exam is growing. On the pediatric front, an estimated 1 in 68 children in the United States has autism spectrum disorder (ASD).1 Moreover, a higher incidence of significant ophthalmologic abnormalities has been found in patients with ASD.2,3
At the Greater Baltimore Medical Center, Mary Louise Z. Collins, MD, embarked on a retrospective study of her pediatric ophthalmology practice after observing an increasing number of ASD patients over the years, many of whom had ocular motility problems. A chart review of 44 ASD patients revealed a higher percentage of patients with strabismus, amblyopia, and anisometropia compared with the general population.
Specifically, 52% had an ocular abnormality, including 41% with strabismus, 27% with significant refractive error, 7% with anisometropia, and 11% with amblyopia.2
“Although our practice has a selection bias—since many more severely affected autistic patients are referred to us for eye exams—and the study was small and retrospective in nature, it does point to the vital need for specialists to examine these nonverbal patients for ocular disorders,” Dr. Collins explained.
Another retrospective chart review, from the Saint Louis University School of Medicine, found ophthalmologic pathology in 40% of patients with autism or a related disorder; conditions included significant refractive errors (29%), strabismus (21%), and amblyopia (10%).3 The authors called for a larger prospective study to obtain the exact incidence of ophthalmologic disorders in these patients, and they urged providers to refer them to pediatric ophthalmologists for eye examinations.
“Simply because a child has a developmental disability doesn’t mean that he or she should have to live with a vision problem, especially since we have come a long way in the past 50 years to visually rehabilitate and mainstream children,” Dr. Collins said. “The nonverbal eye exam is a crucial step in ensuring we are maximizing both their visual and educational potential.”
 |
|
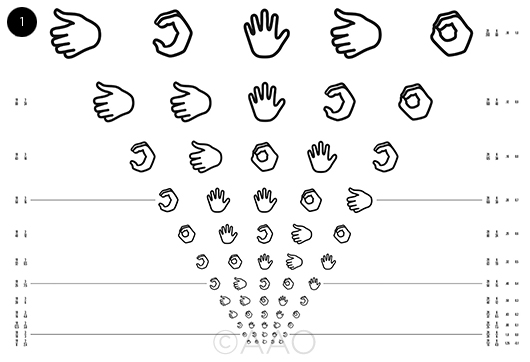
VISUAL ACUITY. Nonverbal patients can use their own hands to replicate the optotypes and indicate recognition.
|
Not Just Pediatrics
The need for nonverbal exams extends well beyond the pediatric population. In addition to evaluating children with ASD, ophthalmologists are called to examine adult patients with cognitive impairment and neurological disorders such as cerebral palsy, muscular dystrophy, and traumatic brain injury. Nonverbal exams can also be used to assess vision in patients who are hearing impaired or—when translation services are not available—those who do not speak the same language as the ophthalmologist.
A New Visual Acuity Test
Given these challenges, Dr. Hutchinson and her colleagues have worked to “expand the armamentarium for eye charts for patients who are nonverbal or don’t speak English.”
Dr. Hutchinson, who has worked for years with multiply disabled children, was approached by a teacher for the visually impaired who had the idea of using Wingdings (symbols developed for computer use) to conduct functional visual assessments. “While the concept was innovative, Wingdings were not a good test of visual acuity,” she said.
Instead, four optotypes—“thumbs-up,” “circle,” “hand,” and letter “C” hand gestures—were created for a new chart, which is known as the Handy Eye Chart (see Fig. 1). The optotypes are “designed to blur equally and are presented in a chart format developed in accordance with accepted standards for visual acuity chart construction,” Dr. Hutchinson explained.
The chart has been validated in a study of 60 verbal children. The children, who were between the ages of 6 and 18, had visual acuities ranging from 20/16 to 20/200.4 The researchers also validated a mobile medical application, Dr. Hutchinson said. The app, called the Handy Eye Check, uses single optotypes presented on a tablet to test visual acuity with the Ambylopia Treatment Study protocol.5 An article comparing the Handy Eye Chart with the Lea Symbols Chart in deaf children was published recently6; another, which compares the new chart with the Landolt C chart, is in preparation.
“Studies have shown that deaf students have high rates of undiagnosed refractive errors, and accurate testing of visual acuity is especially important in these patients, who rely so heavily on vision,” Dr. Hutchinson said. “This eye chart would be a great option.” She added that the chart could be used with nonverbal adults, in instances in which language differences may inhibit visual acuity tests, and, in the hospital setting, with intubated patients of all ages.
Additional Pearls for Nonverbal Exams
Evaluate for nystagmus and strabismus. If a patient adopts a compensatory head position during the exam, nystagmus or strabismus may be an issue. Dr. Collins uses prism lenses to measure strabismus and encourages children 18 months or older to “ride the motorcycle,” having them grasp the slit lamp like handlebars. She also uses handheld slit lamps for developmentally disabled patients.
Use anesthetic eyedrops. Dr. Demer always uses anesthetic drops, as the anesthetic enhances the penetration of dilating eyedrops. And since toddlers are inevitable screamers, he also has soundproof eyedrop rooms to avoid frightening children elsewhere in his office suite.
Consider handheld tonometers. While nonverbal examinations often depend on low-tech, old-school methods, newer devices such as handheld tonometers to measure intraocular pressure are helpful, particularly in younger patients, Dr. Demer said.
|
The Art of the Exam
Nonverbal eye exams have come a long way from the routine use of eye specula and anesthetizing children with chloral hydrate. The following are pearls that Drs. Collins and Demer have gathered via extensive experience.
Begin at the beginning. Patients’ eye movements and behaviors should be observed from the moment they enter the examination room.
Provide distractions. Ophthalmologists who work with nonverbal patients use myriad nontraditional tools to help distract patients, as needed. Dr. Demer noted that the nonverbal eye exam must be tailored to the age and capabilities of the patient. Further, examination rooms must be optimized with what he refers to as “novelty” equipment that both provides visual stimuli and makes the visit fun. As a pediatric ophthalmologist, he has motorized animals activated via foot pedals, video movies controlled by foot pedals, hand puppets, and light-up toys in his suite of 8 examination rooms—along with his ability to wiggle his ears and make bird calls.
Be nonthreatening. Because many nonverbal patients are especially sensitive to touch, clinicians must be careful to approach them in a nonthreatening manner. This allows the physician to complete the exam without triggering any traumatic response in the patient.
“The most important thing to do is approach the patient in a nonthreatening way so you can conduct the exam,” Dr. Collins said. “Some children need multiple visits to complete an exam; it is vital that we don’t push the exam if the child is very apprehensive.” Such an approach may be particularly valuable in follow-up appointments, Dr. Demer noted. Specialists at tertiary referral facilities are often called on to provide second opinions, and if a patient’s initial exam did not go well, it exacerbates the difficulty of further evaluation.
For patients who kick or flail their arms, Dr. Demer conducts many clinical parts of the examination at arm’s length. This is made possible by the use of a retinoscope, “an old-school instrument that allows us to measure refractive error in a minute or so with minimal cooperation,” he said.
Be willing to be creative. The clinician must be willing to be spontaneous, rather than rigid, when determining how best to examine nonverbal patients, many of whom have multiple disabilities, the experts said.
The standard ophthalmic exam depends on a methodical approach, which helps ensure that nothing is missed, Dr. Collins said. But with patients who have developmental disorders, following routine steps often is not possible, she said. “Instead, the focus is on what the patient will allow the ophthalmologist to do in that moment.”
___________________________
1 Christensen DL et al. MMWR Surveill Summ. 2016;65(3):1-23.
2 Black K et al. Strabismus. 2013;21(2):98-102.
3 Ikeda J et al. J Autism Dev Disord. 2013;43(6):1447-1451.
4 Cromelin C et al. Ophthalmology. 2012;119(10):2009-2013.
5 Toner KN et al. J AAPOS. 2014;18(3):258-260.
6 Gorham JP et al. J AAPOS. 2016;20(3):243-246.
___________________________
Dr. Collins is chair of the Department of Ophthalmology, director of Pediatric Ophthalmology and Strabismus, and director of resident education for the ophthalmology residency program at the Greater Baltimore Medical Center. Relevant financial disclosures: None.
Dr. Demer is the Arthur L. Rosenbaum Professor of Pediatric Ophthalmology, professor of neurology, chief of the Pediatric Ophthalmology and Strabismus Division, chair of the EyeSTAR Residency-PhD Program in Ophthalmology and Visual Science, and director of the Ocular Motility Laboratory at the Stein Eye Institute at the University of California, Los Angeles. Relevant financial disclosures: National Eye Institute: S; Research to Prevent Blindness: S.
Dr. Hutchinson is professor of ophthalmology in the Section of Pediatric Ophthalmology and Strabismus at Emory Eye Center in Atlanta. Relevant financial disclosures: Dr. Hutchinson has a proprietary interest in the Handy Eye Chart, which is owned by Emory University and licensed to Groundwork Go LLC.
See the disclosure key at www.aao.org/eyenet/disclosures.