Download PDF
For almost a year, Hannah Mitchell* had been looking in the mirror at a bump on one of her eyelids. Over that time, as the bump became larger, the 41-year-old grew increasingly embarrassed by its appearance and became more and more fed up with fielding questions about it. Adding injury to insult, the bump was now starting to hurt.
We Get a Look
Ms. Mitchell finally made it into our oculoplastics clinic, and we noted that she had a raised lesion along the temporal aspect of her right upper lid. It was red and centrally ulcerated, had heaped-up edges, and was firm and not fluctuant. She told us that the lesion was initially painless and small, but recently it had become tender and large enough to weigh down her upper lid (Fig. 1). She had tried to open the lesion herself several times without success. She also had a past medical history of HIV, and her last absolute CD4 count was 104 in October 2013, but she reported having started and faithfully taking HAART therapy since then.
Apart from the eyelid pathology, her ophthalmologic exam was unremarkable, and she appeared healthy. After this gross examination in the clinic, we were highly suspicious of an eyelid malignancy such as keratoacanthoma, Merkel cell carcinoma, basal cell carcinoma, or squamous cell carcinoma. This differential prompted us to proceed with an excisional biopsy with permanent sections.
 |
|
WE GET A LOOK. The right eye at presentation, one year after the patient first noticed the bump, which was initially smaller and painless.
|
Unexpected Findings
When we got the pathology report, we were expecting to read phrases like “atypia at all levels of the epidermis,” suggesting squamous cell carcinoma, or “nests and lobules of basaloid cells with peripheral palisading,” pointing toward basal cell carcinoma.
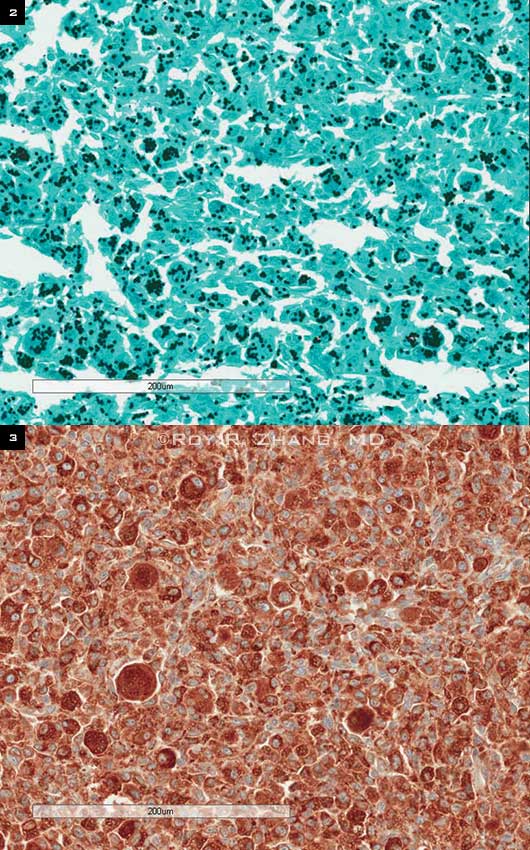
Instead, we read, “Pathology reveals an aggregate of reactive-appearing histiocytes that contain numerous intracytoplasmic yeast on use of H&E [hematoxylin-eosin], GMS [Gomori’s methenamine–silver] stain, and CD68 stains describing the characteristic appearance of histoplasmosis.” Though not initially on our differential, these surprising findings definitively led us to the correct diagnosis of histoplasmosis granuloma (Figs. 2, 3).
 |
|
BIOPSY. (2) GMS stain shows black, dotlike fungal structures intracytoplasmically, consistent with Histoplasma capsulatum (20×, GMS). (3) Immunohistochemical stain of CD68 confirms that the epithelioid cells are histiocytes (20×, CD68).
|
Interesting, but What Next?
Histoplasmosis is an opportunistic mycotic infection that can manifest in cutaneous or visceral form in immunocompromised individuals. It has been considered an AIDS-defining illness since 1987.1 Susceptible individuals can develop a disseminated form, and 10 percent of these can present with cutaneous lesions.2,3 In a study of HIV patients, the patients who developed some form of histoplasmosis infection in any tissue had a median presenting CD4+ count of 94/µl. More importantly, the incidence of histoplasmosis infection sharply increased among patients with CD4+ counts of < 150/µl.4
Because our patient’s history included these factors, which could predispose her to systemic histoplasmosis, we conferred with her infectious disease doctors about the biopsy findings. They felt that her lesion was an isolated cutaneous infection not associated with systemic fungal infection.
Further Discussion
When cutaneous lesions are encountered, disseminated systemic disease should be suspected; however, direct inoculation may also be the etiologic source. Direct inoculation has been reported to cause a primary nodule or indurated ulcer that develops over weeks with or without associated lymphadenopathy, but it is exceedingly rare. Such cases are known as a primary cutaneous histoplasmosis (PCH). In general, mucocutaneous presentation of lesions—involving the mouth, pharynx, and larynx—is more common than cutaneous presentation.5
A cutaneous lesion affords easy access for biopsy, and use of periodic acid–Schiff stain or GMS stain will reveal the 2 to 4 µm intracellular yeast, as proved to be the case in our patient. The tissue may also be cultured with Sabouraud’s agar but may take weeks to grow.5
Histoplasmosis case reports in recent literature include a laboratory technician inoculated through a needlestick,6 a case secondary to trauma in an HIV-positive patient,7 and a case that mimicked an eyelid malignancy, as in our patient.8 However, in the latter case, the lesion presented in the mucocutaneous inferior palpebral conjunctiva versus the epidermal/dermal upper eyelid in our patient. The author of that case also reported two other documented cases of histoplasmosis in the periocular region: The first had massive full-thickness ulceration through the left lower eyelid, and the other had multiple raised lesions along the left upper eyelid that did not raise concern for malignancy. Both of these cases had documented previous systemic histoplasmosis.8
Final Thoughts
Opportunistic infections in the setting of immunosuppression may present in unusual ways. This is a fortunate case in which a suspected cutaneous malignancy was proved to not be a neoplastic process. Furthermore, the infectious etiology was isolated and easily cured with small surgical excision. Reviewing her history and the literature, we hypothesized that the initial etiology was likely either a remote forgotten trauma or an infection after personal drainage attempts. This case reinforces the need for collaboration between specialties as well as the role of medical literature in pinpointing a rare diagnosis and pursuing appropriate management and follow-up.
___________________________
* Patient name is fictitious.
___________________________
1 [No authors listed] Leads from the MMWR. Revision of the CDC surveillance case definition for acquired immunodeficiency syndrome. JAMA. 1987;258(9):1143-1145, 1149, 1153-1154.
2 Hajjeh RA. Clin Infect Dis. 1995;21(suppl 1):S108-S110.
3 Baddley JW et al. Diagn Microbiol Infect Dis. 2008;62(2):151-156.
4 McKinsey DS et al. Clin Infect Dis. 1997;24(6):1195-1203.
5 Smith JA et al. Curr Infect Dis Rep. 2013;15(5):440-449.
6 Buitrago MJ et al. Mycoses. 2011;54(6):e859-e861.
7 Gomez-Moyano E et al. J Mycol Med. 2011;21(3):210-213.
8 Merin MR et al. Ophthal Plast Reconstr Surg. 2011;27(2):e41-e42.
___________________________
Dr. Tan is a third-year resident and Dr. Moreau is an assistant professor of ophthalmology; both are at the Dean McGee Eye Institute in Oklahoma City. They report no related financial interests.