By Lucy Y. Zhang, MD, and Seth W. Meskin, MD
Edited by Steven J. Gedde, MD
Download PDF
Sister Amanda Edwards* started noticing the “black dust” in her eyes about 5 months before she presented to us. The 29-year-old Caucasian nun could see a sprinkling of black specks when she pulled down her lower eyelids, although her eyes felt just fine and her vision was not affected. At first, she thought it was soot or dirt. But when it did not go away, even months later, she became worried and went to see her primary care doctor. She subsequently saw several eye doctors before finding her way to our office.
We Get a Look
When Sister Edwards came to see us, she said the black specks bothered her for cosmetic reasons. There was no discomfort. She had 20/20 vision in both eyes, and no ocular history. She had never worn contact lenses.
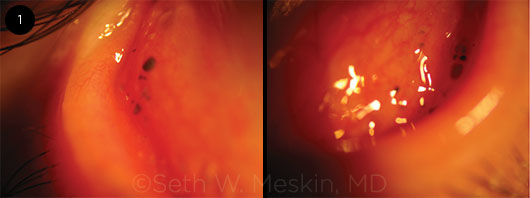
When we pulled down her lower lids, we noted multiple concretions as well as conjunctival cysts; some of the latter were unpigmented and some had black pigmentation. These pigmented lesions were located in the inferior tarsal and forniceal conjunctiva in both eyes, with variable sizes and in no specific pattern (Fig. 1). When we everted the upper lids, we noted only a single concretion. There was no increased vascularization.
The pigmented lesions could not be washed out of the eye nor removed with a cotton-tipped applicator. Apart from the findings on the conjunctiva, the remainder of her eye exam was entirely unremarkable. She did not have any similar lesions on her oral mucosa.
 |
|
BILATERAL CYSTS. We noted that the patient had pigmented and nonpigmented cysts in the inferior palpebral conjunctiva.
|
Her Medical History
The appearance of her conjunctival lesions looked very much like a textbook photograph of adrenochrome deposits. But she claimed that she had never used eyedrops in her life. She had no allergies and no other medical history, and oral doxycycline for acne was the only drug she was taking. Her lifestyle was as expected for a nun—no alcohol, tobacco, or illicit drug use. So what was happening with her eyes? Perhaps these lesions were due to an unknown environmental exposure at the convent, or maybe she had a systemic illness that was not yet diagnosed.
A thorough review of systems was negative. On careful questioning, she did mention that she had been cleaning an old cast-iron stove lately, but she could not recall any specific eye irritation related to the task nor any foreign bodies that had entered her eyes.
Differential Diagnosis
There are several possible causes of acquired pigmented conjunctival deposits or lesions.
Adrenochrome deposits. One classic cause is oxidation of epinephrine drops, which can lead to conjunctival deposits of adrenochrome, a melanin-like pigment accumulation. However, this condition is rarely seen now that topical epinephrine use is very uncommon.
Melanocytic proliferation. In considering pigmented lesions, the differential must include melanocytic proliferation, such as in conjunctival nevi and congenital or acquired melanosis. And although our patient was only 29 years old, we also had to consider the possibility of a malignant process, such as conjunctival melanoma or metastatic tumors from elsewhere.
Other possibilities. The differential should also include:
- Cosmetics deposits
- Encysted environmental irritants (perhaps particles from the cast-iron stove?)
- Foreign bodies
- Hemosiderin deposition following hemorrhage
- Alkaptonuria (metabolic disorder resulting in accumulation of homogentisic acid in connective tissues, where it is oxidized and polymerized into a black pigment)
- Addison disease
- Pregnancy-induced hyperpigmentation
- Argyrosis (discoloration from long-term use of silver-containing solutions)
- Industrial exposure to chemicals, such as aniline dyes and arsenic
- Other drug-induced side effects
In Sister Edwards’ case, with no further clues in her medical history to guide us, we decided to do an excisional biopsy of a few pigmented lesions and sent the sample for pathology.
A Diagnosis Is Made
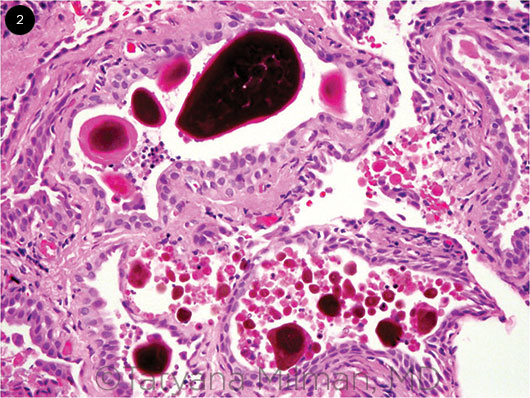
Much to our surprise, and to the patient’s relief, the pathology report came back as conjunctival concretions containing eosinophilic and pigmented acellular material (Fig. 2), which displayed yellow-green autofluorescence. This material did not stain for hemosiderin or melanin, and there was no evidence of malignancy.
The pathologist concluded that these findings were consistent with minocycline/tetracycline-induced conjunctival deposits. And, of course, looking back at the medical history, we noted that doxycycline was the only drug Sister Edwards was taking, so it suddenly all made sense. In fact, she had also been on minocycline at some point in the past 4 years. Fortunately, these deposits are benign. She would have to decide what bothered her more—the black spots on her conjunctiva or the acne on her face.
 |
|
BILATERAL CYSTS. We noted that the patient had pigmented and nonpigmented cysts in the inferior palpebral conjunctiva.
|
Further Discussion
Reports of tetracycline- and minocycline-induced conjunctival pigmentary deposits were published as early as 1981.1
Appearance on exam. Examination typically reveals pigmented and unpigmented conjunctival cysts (often in the lower palpebral conjunctiva), which frequently mimic the appearance of epinephrine-related adrenochrome deposits.
Under light microscopy, the pigmented cysts contain laminated eosinophilic to brownish concretions that show yellow-green autofluorescence. This type of autofluorescence is characteristic of tetracycline-type drugs. The unpigmented cysts contain faintly eosinophilic amorphous material that also display yellow-green autofluorescence. There is an inverse relationship between pigmentation and autofluorescence of the cyst contents.
These pigment deposits are thought to represent an oxidation product of tetracycline-class drugs; they do not bleach, nor do they stain for iron, melanin, or lipofuscin. The epithelial cells that line the conjunctival cysts also lack cytoplasmic pigment granules, such as can be seen in thyroid epithelium following minocycline therapy.2
Although most reported cases of conjunctival deposits have been made through pathology-proven biopsies, 1 report demonstrates autofluorescence of palpebral conjunctival deposits photographed in vivo, which may allow for a diagnosis without biopsy in the appropriate clinical picture.3 Other known side effects of tetracycline compounds include discoloration of the skin, nails, sclera, gum, teeth, bones, and thyroid, but with differing mechanisms of pigment accumulation.
Medications. Of the cases of tetracycline/minocycline conjunctival deposits reported in the literature, all of the patients had been taking these medications orally long-term, between 2½ years and 14 years. Drugs in the tetracycline family—including minocycline and doxycycline—are frequently prescribed for the treatment of acne and rosacea. In ophthalmology, doxycycline is prescribed for the treatment of blepharitis as well as corneal melt and chemical burns.
Conclusion
This case illustrates the finding of pigmented conjunctival cysts in a patient using oral doxycycline, at a dose of 150 mg daily. Given how commonly these drugs are prescribed, it is important for ophthalmologists to be familiar with their ocular side effects and to include drug-induced pigmentation in the differential diagnosis of conjunctival pigmented lesions. Discontinuation of the inciting drug prevents further pigment deposition.
___________________________
* Patient name is fictitious.
___________________________
1 Brothers DM, Hidayat AA. Ophthalmology. 1981;88(12):1212-1215.
2 Messmer E et al. Ophthalmology. 1983;90(12):1462-1468.
3 Lim LT et al. Semin Ophthalmol. 2012;27(1-2):25-26.
___________________________
Dr. Meskin is clinical instructor of ophthalmology, and Dr. Zhang is chief resident; both are at the Department of Ophthalmology and Visual Science at Yale University School of Medicine, New Haven, Conn. Dr. Meskin is also in private practice. Relevant financial disclosures: None.