Download PDF
Highlighted Paper at AAO 2015: Retina
Angiography based on optical coherence tomography (OCT) could be the noninvasive tool ophthalmologists have needed to easily evaluate the level at which macular ischemia is occurring in eyes with diabetic retinopathy, according to researchers in Oregon.
Updated angiography. Unlike traditional angiography, OCT angiography using a specialized processing algorithm can be performed quickly, without the need for intravenous dye injection, said coauthor Thomas S. Hwang, MD. The system that he and his coauthors tested in 12 eyes with diabetic retinopathy and 12 control eyes works by detecting speckle variation in narrow spectral channels, to track the motion of blood through retinal vessels.
“We’re excited about the ability to automatically quantify macular nonperfusion using this technology,” said Dr. Hwang, who is an associate professor in the Retina Division of the Casey Eye Institute of Oregon Health & Science University (OHSU) in Portland.
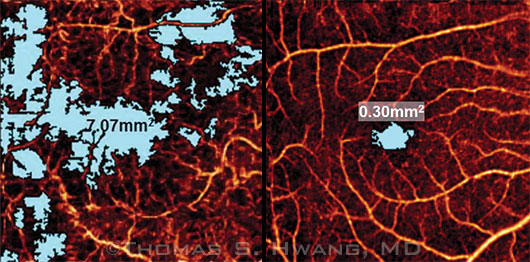 |
Comparative Vascularity. (Left) 6×6-mm OCT angiogram of an eye with diabetic retinopathy shows an avascular area (blue) covering a total of 7.07 mm2. (Right) The nonperfused area measured in a normal macula is 0.30 mm2.
|
New algorithm speeds the process. The use of OCT for angiography has been studied since 2006, but the early experimental systems were time-consuming and clinically impractical because they required multiple and repeated scans of each location to build the angiogram. In the current study, the researchers speeded up the process by using a split-spectrum amplitude-decorrelation angiography (SSADA) algorithm, which was developed at OHSU.1 With SSADA, angiography of the macula takes about 3 seconds because only 2 scans are required at each location, Dr. Hwang said. The 3-dimensional flow signal over the central 6×6-mm area is then presented as an en face angiogram, and an automated algorithm can compute the total area of avascularity.
| Automated Quantification of Macular Ischemia Using OCT Angiography in Diabetic Retinopathy. When: Monday, Nov. 16, 4:16-4:23 p.m., during the second retina, vitreous original papers session (2:00-5:00 p.m.); there is also a session on Sunday. Where: Bassano 2701. Access: Free. |
Revealing retinopathy characteristics. The OCT angiograms in their study showed that, compared with the 12 controls, the 12 eyes with diabetic retinopathy had reduced parafoveal and perifoveal vessel density (p < .001), a larger macular avascular area (p < .001), and a larger total foveal avascular zone (p = .057), Dr. Hwang said. Furthermore, the macular avascular area measurements identified diabetic retinopathy with 100% sensitivity and specificity, he said.
“We have known for a long time that macular nonperfusion is an important indicator of prognosis, but grading the degree of nonperfusion has been tedious and difficult at best and very subjective at worst. Clinically, doing the kind of grading that the ETDRS study did is impractical.” He added, “Our study shows that it might be feasible to have a detailed and objective evaluation of the macular circulation that could be used in real clinical practice.”
—Linda Roach
___________________________
1 Jia Y et al. Proc Natl Acad Sci USA. 2015;112(18):E2395-E2402.
___________________________
Relevant financial disclosures—Dr. Hwang: None
For full disclosures and disclosure key, see below.
More from this month’s News in Review