By Tayler M. Schwartz, SCB, Robert T. Keenan, MD, MPH, and Melissa B. Daluvoy, MD
Edited by Sharon Fekrat, MD, and Ingrid U. Scott, MD, MPH
Download PDF
Rheumatoid arthritis (RA) is an autoimmune disease that classically presents with symmetrical inflammatory polyarthritis, joint stiffness, fever, weight loss, and malaise. There may also be periarticular bony erosions, joint deformities, and nodules, with classic sparing of the distal interphalangeal joints. Females are more commonly affected, and there is an association with human leukocyte antigen (HLA)-DR4 and increased cytokine Th17. RA has diverse extra-articular manifestations, including in the cardiac, pulmonary, nervous, renal, skeletal, circulatory, and ocular systems.
Diagnosis
Diagnosis of RA is based on joint involvement, symptom duration, and serum studies, including rheumatoid factor and anti–cyclic citrullinated protein (the most specific marker). Evaluation may also include joint radiographs and complete blood count with differential, C-reactive protein level, and erythrocyte sedimentation rate. Uric acid level and liver and kidney function tests can help exclude other etiologies or guide medication dosing.
Pathophysiology
Like the joints, the sclera and cornea contain proteoglycans and collagen. This histologic similarity likely accounts for many of the ocular manifestations of RA. The ocular conditions associated with RA have pathological features in common with vasculitis, which may include vascular occlusion, infiltration, and fibrinoid necrosis. Processes at play include immune complex deposition, secretion of collagenases (e.g., matrix metalloproteinases) by macrophages and neutrophils, cytokine production, complement activation, and formation of autoantibodies.1
Dry Eye Syndrome
Dry eye syndrome, also known as keratoconjunctivitis sicca, is the most common ocular manifestation of RA. It can occur as a result of meibomian gland, lacrimal gland, accessory lacrimal gland, or goblet cell dysfunction.
Characteristics. Symptoms of dry eye syndrome include foreign body sensation, burning, decreased visual acuity, photophobia, and pruritus.
Diagnostic signs include less than 5 mm of tear extension on Schirmer’s test, tear break-up time of 5 seconds or less, decreased lacrimal lake, and staining with fluorescein, rose bengal, or lissamine green.1 Up to 25% of patients with RA meet criteria for secondary Sjögren syndrome, which is less commonly associated with xerostomia than is primary Sjögren syndrome. Notably, different HLA genes are associated with primary Sjögren syndrome and Sjögren syndrome secondary to RA.2 Additionally, the prevalence of positive anti-Ro antibodies and anti-La antibodies is low in patients with RA, found in one study to be 12.2% and 11.3%, respectively.3
Other considerations. The normal tear film has antimicrobial properties and contains immunomodulatory factors such as collagenase inhibitors (e.g., alpha-2 macroglobulin). Patients with dry eye syndrome are deficient in these protective mechanisms and have increased proteolytic enzymes such as plasminogen activator in the tear film.4 Consequentially, dry eye syndrome can lead to superficial punctate keratitis, filamentary keratitis, corneal ulcer, and ultimately, corneal melt.1 Accordingly, RA is a relative contraindication against refractive surgery, especially LASIK, due to its potential to exacerbate dry eye syndrome.4 (See also “Surgical Considerations in RA Ocular Disease.”)
Treatment. Therapeutic modalities include lubricating drops and ointments, topical cyclosporine, and oral pilocarpine. The recent approval of lifitegrast has added a new medication to our armamentarium of topical treatments. In-office procedures include punctal occlusion, use of amniotic membrane, and tarsorrhaphy.
Episcleritis
Episcleritis is inflammation of the episclera, which lies just beneath Tenon’s capsule. Although the disorder is usually idiopathic, it can also be associated with RA and other systemic diseases. It is bilateral 40% of the time, and manifests with salmon-pink eyes and mild pain. It can occur sectorally in a radial distribution; in a diffuse pattern; and, less commonly, in a nodular form. In contrast to scleritis, eye redness resolves with topical phenylephrine.
Treatment. Episcleritis is usually self-limiting. Topical corticosteroids or oral nonsteroidal anti-inflammatory drugs (NSAIDs) can be used for symptomatic relief.
Scleritis
RA is the most common cause of scleritis, which is an inflammation of the sclera characterized by vasodilation of the superficial and deep episcleral vessels. Occasionally, scleritis may present before the onset of joint symptoms in the RA patient. It may also occur as a manifestation of systemic vasculitis. Scleritis occurs bilaterally 40% to 50% of the time and is classified as anterior or posterior based on its position relative to the ora serrata.
Types of scleritis. Anterior scleritis can be nodular, diffuse, or necrotizing. It usually presents with intense pain amplified by eye movements, blurry vision, photophobia, and tearing (Fig. 1).
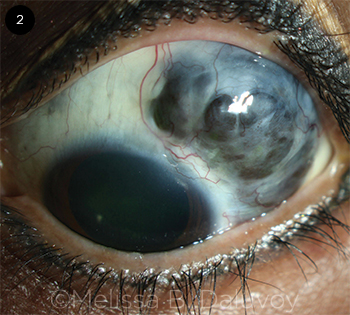
Scleromalacia perforans describes anterior necrotizing scleritis without inflammation (Fig. 2). This condition often presents without pain, despite its ability to lead to visual loss, astigmatism, and globe perforation.
Posterior scleritis is characterized by the “T” sign on B-scan. This classic sign is produced by hyporeflectivity from both the optic nerve and fluid under Tenon’s capsule.
 |
|
ANTERIOR SCLERITIS. Slit-lamp photo displays dilation of the episcleral vessels in a patient with underlying RA.
|
Other considerations. The presence of scleritis in patients with RA is associated with increased mortality.1 Posterior scleritis can cause serous retinal detachment or chorioretinal folds. Other sequelae associated with scleritis include uveitis, cataracts, glaucoma, posterior segment damage, and peripheral ulcerative keratitis.
Treatment. Topical medications are generally not effective in the treatment of scleritis. Therapy should focus on managing the underlying RA, with a multidisciplinary team approach involving the patient’s primary care physician and rheumatologist. Oral NSAIDs are most effective in mild cases and for nodular anterior scleritis.
For more severe disease, the treatment of choice is oral corticosteroids (1 mg/kg/day of prednisone equivalents), with an optional bolus of methylprednisolone 1 g daily for 3 days.
Depending on response and severity of scleritis at presentation, additional systemic medications include methotrexate, azathioprine, mycophenolate mofetil, cyclosporine, and biologic agents such as infliximab, adalimumab, rituximab, and anakinra. Immunologic agents, most commonly intravenous or oral cyclophosphamide, can be added for necrotizing disease and refractory cases.1
For necrotizing scleritis, exploration and debridement with tectonic patch grafting may be necessary for severe thinning or perforation.4
 |
|
SCLEROMALACIA PERFORANS. Slit-lamp photo of the left eye shows severe superotemporal scleral thinning with visible choroid bulging anteriorly, but with minimal inflammation.
|
Peripheral Ulcerative Keratitis
Peripheral ulcerative keratitis (PUK) is a type of corneal melt that occurs when immune complexes infiltrate the vascular arcades in the 0.5-mm corneal periphery. RA is the most common etiology, accounting for 34% of cases; however, it can also be caused by other autoimmune, infectious, neurologic, and dermatologic conditions.5 In the setting of severe RA, PUK is usually accompanied by other ocular manifestations, and it can occur secondary to scleritis, especially necrotizing scleritis.1,5
Characteristics. PUK presents with stromal thinning and a secondary overlying epithelial defect and is characterized by neovascularization of the corneal periphery and crescent-shaped juxtalimbal ulcers (Fig. 3).5 It is unilateral 60% of the time.1 It can present with pain, photophobia, tearing, and decreased visual acuity due to astigmatism or corneal opacity.
The differential diagnosis includes Mooren ulcer, Terrien marginal degeneration, herpetic keratitis, corneal ulcer secondary to dry eye, phlyctenular ulcers, and marginal keratitis. Corneal perforation is a feared complication.
 |
|
PUK. Crescent-shaped ulcers are juxtaposed against the limbus.
|
Other considerations. Like necrotizing scleritis, PUK is associated with increased mortality in patients with RA, and it can be a sign of impending systemic vasculitis.1
Treatment. The treatment strategy should prioritize management of the underlying RA. Systemic corticosteroids with or without immunologic agents are the mainstay of treatment. These agents may include oral mycophenolate mofetil, methotrexate, azathioprine, leflunomide, infliximab, adalimumab, or rituximab. Oral cyclosporine can be used if there is no underlying systemic vasculitis. Oral cyclophosphamide can be used in cases unresponsive to treatment, while etanercept is less effective.
Ocular support. Additional measures to help protect the cornea include topical medroxyprogesterone and acetylcysteine, which act as collagenase inhibitors, and oral tetracycline, which inhibits matrix metalloproteinase.5
Treating coexisting dry eye syndrome can bolster the tear film to conserve corneal integrity and prevent keratolysis. However, topical steroids can increase risk of perforation and should be avoided.2 Tissue adhesives such as cyanoacrylate glue; amniotic membrane; bandage contact lenses; and tectonic, lamellar, or penetrating keratoplasty can be used to prevent and manage perforation.
Although controversial, perilimbal conjunctival resection may remove the immune complexes at their entry point into the cornea.5
Surgical Considerations in RA Ocular Disease
Surgical trauma can initiate macrophage and neutrophil infiltration, resulting in a progressive immunologic response and the deposition of immune complexes. When deposited in the cornea, these immune complexes contribute to a keratolytic response. During the initial inflammatory process, fibroblasts are recruited and activated, producing complement component C1 and contributing to the activation of the classical complement cascade. The surgical trauma itself may compromise ocular immune privilege and incite immune responses due to molecular mimicry.
Additionally, the risk of postsurgical sterile corneal melt is higher in the setting of RA and coexisting dry eye syndrome, so treatment of the RA and surface disease should be optimized prior to any ocular surgery. Perioperative oral prednisone should be considered in patients with known RA. If necrotizing scleritis occurs after ocular surgery without known underlying RA or other systemic collagen vascular diseases, these entities should be suspected.1
___________________________
1 Perez VL et al. Semin Ophthalmol. 2002;17(3-4):124-130.
|
Key Points
Ocular manifestations of RA include dry eye syndrome, episcleritis, scleritis, and PUK. The most vision-threatening sequelae include corneal perforation or ruptured globe from scleritis, particularly scleromalacia perforans. Multidisciplinary management is important, especially in the presence of scleritis and peripheral ulcerative keratitis, which are associated with increased mortality in patients with RA.1
Plaquenil Caveats
Hydroxychloroquine (Plaquenil), a drug used to treat RA or other autoimmune diseases, is linked with a rare, but irreversible, retinopathy. The risk of toxicity depends on dose and duration. If you have patients who take this drug, be sure to consult the Academy’s updated clinical statement on screening recommendations to prevent vision loss.
|
___________________________
1 Artifoni M et al. Nat Rev Rheumatol. 2014;10(2):108-116.
2 Antero DC et al. Rev Assoc Med Bras. 2011;57(3):319-322.
3 Schneeberger E et al. Clin Rheumatol. 2008;27(4):517-519.
4 Perez VL et al. Semin Ophthalmol. 2002;17(3-4):124-130.
5 Yagci A. Clin Ophthalmol. 2012;6:747-754.
___________________________
Ms. Schwartz is a medical student at Brown University. Dr. Keenan is an associate professor of medicine, and Dr. Daluvoy is an assistant professor of ophthalmology; both are at the Duke University School of Medicine. Relevant financial disclosures: None.