Download PDF
Were you in practice back in the mid-80s? If so, you may be experiencing déjà vu.
In 1985, the United States allowed Medicare-funded cataract surgery to be performed on an outpatient basis and adjusted its reimbursement schedule accordingly. This ruling ushered in the era of ambulatory surgery centers (ASCs), transforming cataract surgery from an inpatient hospital-based operation to an outpatient procedure performed in either hospital outpatient departments (HOPDs) or freestanding ASCs.
Now, 3 decades later, the Centers for Medicare & Medicaid Services (CMS) is revisiting the issue of cataract surgery site of service—this time looking into office-based surgery. In 2015, CMS attracted nationwide attention from ophthalmologists when it issued a Request for Information about “nonfacility” (i.e., office-based) cataract surgery in its 2016 Medicare Physician Fee Schedule Proposed Rule.
In this request, CMS stated, “Advancements in technology have significantly reduced operating time and improved both the safety of the procedure and patient outcomes. We believe that it is now possible for cataract surgery to be furnished in an in-office surgical suite, especially for routine cases.”1
CMS subsequently received 138 comments from practitioners and stakeholders from professional medical societies, the RUC (Relative Value Scale Update Committee), ASCs, and the general public. In its final rule after the comment period, CMS noted that many commenters expressed concerns about safety, and others suggested the development of PE RVUs (Practice Expense Relative Value Units) appropriate for the office setting to allow for greater flexibility regarding scheduling and location.2
The bottom line? CMS “will use this information as we consider whether to proceed with development of nonfacility PE RVUs for cataract surgery.”2
While the definitive rule making had not been published at the time this story was written, the CMS Request for Information opened fresh debate on the optimal setting for cataract surgery—placing issues related to patient safety and facility staffing, costs, reimbursement, and operational efficiency at the center of the discussion.
Medicare’s Quest to Lower Costs
Michael X. Repka, MD, MBA, the Academy’s Medical Director for Government Affairs, noted that the CMS Request for Information on office-based cataract surgery reflects Medicare’s push to move surgery to the lowest-cost setting that is considered medically safe.
“This is a logical consideration given that cataract surgery is the most common Medicare operation in the United States, with 1.6 million procedures performed annually under Medicare Part B alone,” Dr. Repka said. “Consequently, any ruling regarding the site-of-service delivery would potentially have an enormous impact on ophthalmology.”
Added David F. Chang, MD, who is in private practice in Los Altos, Calif., “The volume of cataract surgery will dramatically increase as our population ages. Many ophthalmologists therefore suspect that the motivation behind this initiative is to reduce overall CMS expenditures for cataract surgery.”
Lesson from history. Dr. Chang noted that as the majority of cataract surgical volume was moved from HOPDs into ASCs, the profession saw a significant reduction in facility reimbursement without any real reduction in the procedural costs of doing the surgery.
“Compared to HOPDs, ASCs have the same costs for equipment, supplies, drugs, staff, and administrative paperwork for cataract surgery; and the regulatory requirements are no less costly or burdensome,” Dr. Chang said. “In fact, CMS surveyors have imposed stricter regulations that have universally increased ASC overhead and costs compared with a decade ago. Despite these facts, ASC cataract surgery reimbursement remains significantly lower than that for HOPDs, resulting in enormous savings for CMS.”
Yet ASCs remain profitable, said Dr. Repka, “because they are spectacularly efficient.” ASC-based surgeons can do 3 to 4 times more cases per hour than those in a hospital setting, making ASC overhead less per capita than at a hospital, he said.
Compromising patient safety? Given the efficiency of ASCs and the rigid regulatory requirements, Dr. Chang said, it is “hard to understand” how in-office cataract surgery would reduce facility costs unless the CMS applies different licensure standards for the facilities. And, he said, “It is also hard to imagine CMS accepting or sanctioning double standards for patient safety.”
Is Office-Based Cataract Surgery Safe?
Patient safety is always a top concern when considering rule changes. One large study that looked into the safety and effectiveness of office-based cataract surgeries garnered much interest last year.3
The findings. This retrospective review of 21,501 eyes (13,507 patients, aged 72.6 ± 9.6 years) undergoing office-based cataract surgery in Kaiser’s Denver metropolitan area between 2011 and 2014 found good visual outcomes with a safety profile “well within expectations for modern cataract surgery.”3
Specifically, 15 cataract surgeons performed phacoemulsification with intraocular lens (IOL) implantation in 99.9% of eyes and manual extracapsular cataract extraction in 0.1% of eyes. The authors wrote, “Overall vision outcomes were excellent with mean postoperative best-corrected visual acuity of 20/28 Snellen, and surgical reintervention was required in only 0.6% and 0.7% of patients at 3 and 6 months postoperatively, respectively.”
Complications. Lead author Tsontcho “Sean” Ianchulev, MD, MPH, at the University of California, San Francisco, said he was surprised that there were not more complications, given the age of the population and comorbidities, which included hypertension, diabetes, and chronic obstructive pulmonary disease. Intraoperative adverse events included 119 (0.55%) cases of capsular tear and 73 (0.34%) cases of vitreous loss. Postoperative adverse events included 330 (1.53%) cases of iritis/ uveitis, 110 (0.53%) cases of corneal edema, and 30 (0.14%) cases of retinal tear or detachment. “We couldn’t find one case of endophthalmitis,” he noted.
The goal. He added that the investigators were conducting academic population health research to assess the safety of the Kaiser experience. “Kaiser’s several years of experience in office-based cataract surgery by multiple surgeons, documented through an extensive electronic medical records system, compelled us to analyze this treasure trove of data in terms of safety and efficacy,” he noted.
“This study illustrates the power of big data and the insight we can gain from real population health studies,” Dr. Ianchulev said. “It also adds to the discussion of how we can do cataract surgery safely and efficiently.” He noted that the study demonstrates that the operation could be performed safely in an office-based setting using the same equipment, procedures, and antibiotics as implemented at Kaiser.
Kaiser advantages. However, the Kaiser experience may not be transferrable to typical in-office surgery setups. For instance, the Kaiser study included safety protocols that other offices might not be able to provide.
- A crash cart with “Nurse Stat” team was on standby to handle any life-threatening complications.
- Office suites were located no farther than 1.5 km from a Kaiser-affiliated hospital.
In addition, said Dr. Ianchulev, a large health system can create certain controls and efficiencies. For example, Kaiser can select patients to have office-based surgery and allow higher-risk patients to have more monitoring in an ASC or in a hospital.
Concerns About Safety
Steven I. Rosenfeld, MD, at Delray Eye Associates in Florida, said that safety is a source of trepidation when considering shifting to office-based cataract surgery. “It takes a great level of skill to perform cataract surgery, and there is not a large margin for error when operating on the eye.” But he observed that ophthalmologists have “shot themselves in the foot by touting for decades how quickly we can perform a cataract operation. It depreciates the value of what we do and gives the impression—especially to CMS—that this must be a simple, routine operation.”
Few routine cases. Michael A. Romansky, JD, Washington Counsel representing the Ophthalmic Outpatient Surgery Society (OOSS), pointed to a CMS assertion that he calls misguided: “… it is now possible for cataract surgery to be furnished in an in-office surgical suite, especially for routine cases.” In August 2015, OOSS, in cooperation withthe Association of Ambulatory Surgery Centers and the Society for Excellence in EyeCare (SEE), involved 170 ophthalmic ASCs in a study to randomly sample the medical records of 50 of their most recent cataract patient cases. The study found that “routine” cases are rare, as “virtually all of our patients present with multiple comorbidities.” Specifically, the OOSS study found that 94% of cataract patients presented with 1 or more comorbid conditions, including hypertension, cardiovascular disease, cerebrovascular disease, pulmonary disease, endocrine disease, and cancer.
In its official 20-page response to the CMS Request for Information,4 OOSS stated that “in terms of identifying ‘routine’ cataract cases, only 6% of cataract cases present without any comorbidities, and most are taking multiple prescription medications associated with comorbidities. Thus virtually all cataract patients are potentially at risk unless their surgery is performed in office facilities that meet standards of care comparable to those of ASCs and hospitals.”
Rigorous standards needed. Mr. Romansky noted that 30 years ago, many ASCs looked like physician offices. Today, because of strict regulations and a commitment to safety and quality, ASCs are “sophisticated facilities that have made extensive investments to keep patients safe.”
In addition, OOSS addressed every ASC regulatory standard, stressing that all of them need to be applied to physician offices. “We addressed the surgical environment, ASC Life Safety Code, infection control, surgical services such as anesthesia, nursing, patient assessment, administration and oversight of drugs, and medical records,” Mr. Romansky said. “We urged CMS, before implementing payments for office surgery, to develop standards of care for office facilities that are similar to those applied to ASCs.”
Implementation issues. Brock K. Bakewell, MD, who has an ASC in Tucson, Ariz., said he is concerned about standards of care if Medicare starts allowing office-based cataract surgery. “How will CMS oversee Medicare’s Conditions for Coverage, including quality improvement, quality assurance, and peer review? How will they retain all of the same strict standards that ASCs must adhere to?
“If the standard of care in an office is lower than in an ASC, this concept won’t work,” Dr. Bakewell continued. “And if Medicare doesn’t inspect the office practices and quality of care declines, we may see worse patient outcomes.”
Anesthesia Services
Dr. Rosenfeld raised a concern about the Kaiser study: Minor procedure room (MPR) staff did not include an anesthesiologist or nurse anesthetist. (The Kaiser authors wrote: “No anesthesiologist is present, and no intravenous lines or injections are routinely used. Only topical ± intracameral anesthesia is generally used, with oral triazolam sedation.”3)
“In my experience, you want to have anesthesiology personnel present,” said Dr. Rosenfeld, citing a study that he conducted using data gathered from his surgery center in Boca Raton, Fla., which found that more than one-third of cataract surgery cases required anesthesia intervention.5 The study evaluated the incidence of intervention by anesthesia personnel to determine the need for monitored anesthesia care in cataract surgery.In 1,006 consecutive cataract surgery cases, intervention by anesthesia personnel was required in 376 (37.4%) cases. There were no preoperative characteristics that were predictive of the need for intervention, including preexisting medical conditions, abnormal baseline EKG, and patient sex or age.
Safety net. Dr. Bakewell added that at an ASC, the surgeon can handle the full range of cases, from “routine” patients to those with multiple comorbidities. “If a routine patient has an intraoperative complication that requires deeper sedation, it’s nice to know that the patient isn’t being compromised, since an anesthesiologist is always present in the facility to provide the optimal level of sedation and analgesia,” he said.
Dr. Rosenfeld concurred, saying, “Cataract surgery patients do not even have to experience a life-threatening condition to be a challenge for the ophthalmologist. The surgeon has his or her hands full without needing to worry about an anxious patient, hypertension, respiratory depression, bradycardia or other arrhythmias, etc.”
Jonathan M. Davidorf, MD, who operates at an ASC in West Hills, Calif., noted that although most patients can do fine with local anesthesia and diazepam (Valium), the Kaiser study did not take into account those who need a higher level of anesthetic intervention, he said.
Lisa F. Rosenberg, MD, who operates at Northwestern Memorial Hospital in Chicago, cited similar concerns, noting that in-office surgery would be safest when limited to low-risk cataract surgery cases. She defined these as patients who do not have important ocular findings or comorbidities that put them at unacceptable high risk for in-office surgery and who have the ability to remain calm during surgery. She estimates that she is correct 95% of the time in her assessment of which surgeries are high and low risk. “This means that 5% of the time, a patient becomes more anxious or feels more sensation during the surgery than I had expected, so they would need anesthesia.”
Facility Considerations
Dr. Bakewell said he had the option of building his own office-connected ASC because Arizona is not a Certificate of Need state. “For ophthalmologists in Certificate of Need states who want to operate an independent surgery center, their only option may be an office-based surgery suite,” Dr. Bakewell said. “But at this point, Medicare won’t pay the facility fee, just the physician’s fee, for office-based cataract surgery, so how can the physician afford to do surgery in the office? Some surgeons currently performing office-based cataract surgery can afford to do so by only doing premium IOL cases.”
Upsides of MPRs. This could change if CMS were to fully reimburse the costs for in-office cataract surgery. Dr. Ianchulev said that surgeons who do not currently have access to an ASC and, therefore, must perform all surgeries in an HOPD might find that in-office procedures can speed scheduling of patients for surgery and—possibly—eliminate the need for and associated costs of some preoperative laboratory evaluations, establishment of intravenous access, and an anesthesiologist. Dr. Repka added that such a shift might also protect them from some penalties in the Cost component of MIPS.
Dr. Rosenberg agreed that from a logistics standpoint, an MPR is more convenient and could allow for greater efficiency. “Because you wouldn’t have to travel to a different building and because it would all be under your control, you could see more patients and do more surgery—you could deliver more care in general.”
Downsides of HOPDs. Although her office is physically attached to the hospital outpatient department so that getting to and from surgery is not a big issue, she noted that there are some inefficiencies. For example, there is turnover time between cases because the surgeon cannot use 2 rooms. Also, some hospital procedures can be time-consuming—from preoperative clearance and bloodwork in some cases (“which has been shown not to impact low-risk cataract surgery cases”) to postoperative instructions and more, she said.
Financial and Efficiency Hurdles
ASC reimbursement for cataract surgery remains significantly lower than that for HOPDs. Dr. Chang noted that CMS savings would undoubtedly result if physician offices accepted lower facility reimbursement compared with ASCs.
Economic disadvantage. “However,” said Dr. Chang, “the financial risks [for the practice] of doing so would be high. That’s because the cost of supplies and equipment would be just as high, and most offices would not enjoy the efficiencies and economies of scale that ASCs achieve by having multiple surgeons performing higher aggregate volumes.”
A case in point. For Dr. Rosenberg’s practice with 3 other anterior segment surgeons, it would be cost-prohibitive to set up an MPR. “A surgical microscope alone could cost $60,000. It would cost tens of thousands of dollars, or more, for the beds, medications, instruments, lens implant stock, and staffing,” she said, adding that questions of malpractice coverage and reimbursement are further wild cards. “You’d need multiple practices or a multispecialty group so that you have many surgeons paying for it. The costs are almost a nonstarter for a small practice like ours,” she said.
Regulatory burden. Dr. Davidorf added that the regulatory burden—ranging from credentialing processes to requirements for medicated eyedrop administration and more—can at times benefit patient care and at times be seen as a hindrance.
“The mechanics of cataract surgery, or an appendectomy for that matter, can be done in a tent in the desert,” he said. But building out a surgical suite is another matter. “To buy and upgrade equipment is an expense. And the nursing staff and technicians would all need to be cross-trained and paid accordingly,” Dr. Davidorf noted. “You also need the space to store an inventory of lens implants; you need procedures and equipment for sterilizing instruments.
“All in all, to be safe and efficient, the minor procedure room–style of cataract surgery ends up looking like, and acting like, an ASC. If done properly, and in the patient’s best interest, the only thing that changes is the name,” Dr. Davidorf said.
ASCs already are efficient. “If CMS is looking for efficiencies, it won’t find them in an office-based system,” Dr. Davidorf said. “Surgery centers have already found a way to accomplish this—to get a lot of patients safely through the procedure despite extensive regulations. I don’t see how you can provide the same efficiencies or level of service at a savings in the office environment.”
Exceptions? Although the business outlay would be unmanageable for her own practice, said Dr. Rosenberg, “perhaps for a large practice in an underserved area, in-office cataract surgery could make an impact.”
More Evaluation Is Needed
So where does the profession go from here? Dr. Repka said that it is “clearly possible” for cataract surgery to be done in a physician’s office. He suggested that a comparison study be funded to evaluate office-based cataract surgery in the private practice setting versus cataract surgery done in an HOPD or ASC. “This would help us be certain this procedure can be done safely and efficiently in a doctor’s office, as well as define the true costs,” he said.
For office-based surgery to be successful, he added, CMS has to provide enough money for the practice expenses to make it feasible, while having strict regulations in place for safety. “This can’t be done on the cheap,” said Dr. Repka. “And not everyone can afford to equip an office-based surgical suite.”
However, these financial concerns are similar to those that were expressed decades ago when CMS wanted to shift cataract surgery from an inpatient to an outpatient procedure, he said. “Yet we have always been able to develop good quality care along with patient safety, given the right tools and adequate payment,” Dr. Repka said.
He concluded, “Ophthalmology needs to be open to this. Our profession has a history of successfully making similar transitions, and we should be prepared to look closely at it and to determine if it is safe for our patients. We shouldn’t adopt it because it is cheaper, but only if it is safe with high quality, is convenient, and saves money for the health care system.” However, he added, CMS cannot cut corners on payment or no ophthalmologist will be able to provide such a service.
___________________________
Editor’s Note: CMS declined providing a spokesperson to comment on this article, stating CMS is “unable to accommodate an interview on this topic.”
___________________________
1 Medicare Program; Revisions to Payment Policies under the Physician Fee Schedule and Other Revisions to Part B for CY 2016, pages 53-54.
2 Medicare Program; Revisions to Payment Policies Under the Physician Fee Schedule and Other Revisions to Part B for CY 2016 – Final Rule.
3 Ianchulev T et al. Ophthalmology. 2016;123(4):723-728.
4 http://ooss.org/wp-content/uploads/FINAL-2017-ASCRS-OOSS-SEE-ASC-Rule-Comments.pdf.
5 Rosenfeld SI et al. Ophthalmology. 1999;106(7):1256-1261.
Meet the Experts
Brock K. Bakewell, MD In private practice at Fishkind, Bakewell, Maltzman, Hunter and Associates Eye Care & Surgery Center, Tucson, Ariz; adjunct associate professor at the University of Utah; and clinical instructor of ophthalmology and vision science at the University of Arizona, Tucson. Relevant financial disclosures: Fishkind, Bakewell, Maltzman, Hunter and Associates Eye Care & Surgery Center: O.
David F. Chang, MD Cataract specialist in private practice in Los Altos, Calif., and clinical professor of ophthalmology, University of California, San Francisco. Relevant financial disclosures: Peninsula Eye Surgery Center: O.
Jonathan M. Davidorf, MD Director of the Davidorf Eye Group in West Hills, Calif.; and assistant clinical professor at UCLA Jules Stein Eye Institute. Relevant financial disclosures: West Hills Surgical Center, West Hills, Calif.: O.
Tsontcho “Sean” Ianchulev, MD, MPH Clinical associate professor of ophthalmology at the University of California, San Francisco. Relevant financial disclosures: None.
Michael X. Repka, MD David L. Guyton, MD, and Feduniak Family Professor of Ophthalmology at the Wilmer Eye Institute at Johns Hopkins in Baltimore; Academy Medical Director for Governmental Affairs. Relevant financial disclosures: American Academy of Ophthalmology: S.
Michael A. Romansky, JD Washington Counsel for the Outpatient Ophthalmic Surgery Society (OOSS). Relevant financial disclosures: OOSS: E.
Lisa F. Rosenberg, MD Associate professor of clinical ophthalmology, Feinberg School of Medicine, Northwestern University. Relevant financial disclosures: None.
Steven I. Rosenfeld, MD Cornea and cataract specialist in private practice with Delray Eye Associates, Delray Beach, Fla.; and voluntary professor on the clinical faculty at the Bascom Palmer Eye Institute, University of Miami School of Medicine. Relevant financial disclosures: Boca Raton Outpatient Surgery & Laser Center: O.
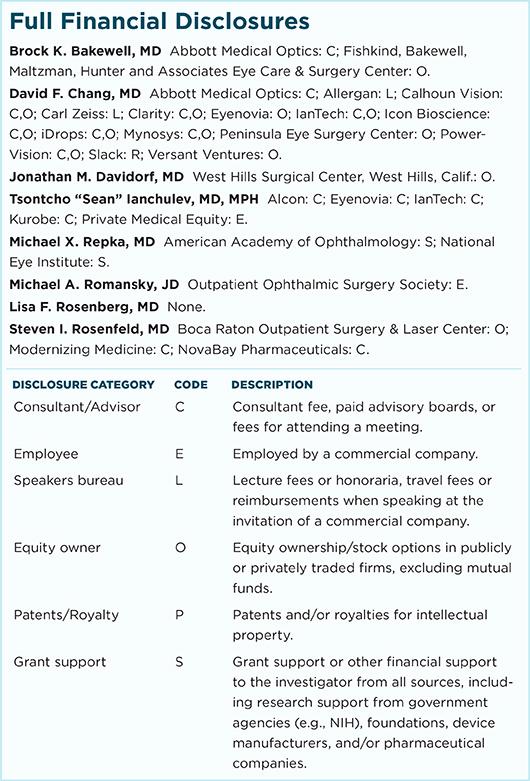
For full disclosures and the disclosure key, see below.
|