Ologen Implant After Trabeculectomy
By Jean Shaw
Selected By: Henry D. Jampel, MD
Journal Highlights
Ophthalmology Glaucoma, September/October 2018
Download PDF
Does the biodegradable collagen matrix implant (Ologen) further the success of trabeculectomy? Findings from the first randomized controlled trial to address this question indicate that it does not.
Sen et al. set out to compare the success of trabeculectomy performed with and without the Ologen implant, which is being investigated as a substitute or an adjunct for antimetabolites such as mitomycin C (MMC).
For this study, the researchers recruited 50 patients (50 eyes), all of whom were Asians from north India, and assigned them to undergo either trabeculectomy with low-dose MMC (1 mg/mL, administered for 1 minute) alone or trabeculectomy plus low-dose MMC and the Ologen implant. The primary outcome was the percentage reduction in intraocular pressure (IOP); secondary outcomes included the percentage of patients achieving absolute and qualified success for IOP <15 mm Hg and <18 mm Hg; the postoperative need for glaucoma medications; and the rate of postsurgical complications.
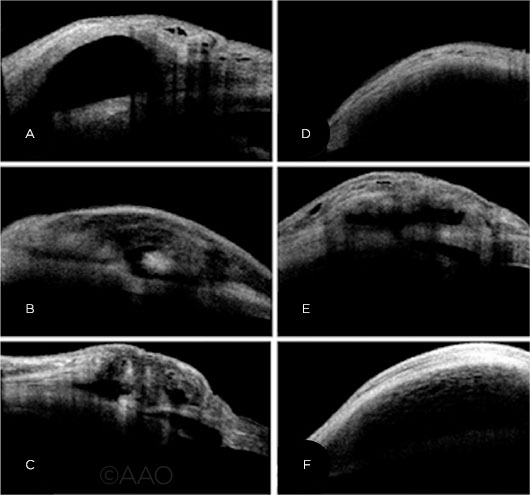 |
BLEB ANALYSIS. All images on the left are of patients who received MMC alone; images on the right are of those who received MMC and the Ologen implant. No side effects linked to the implant were noted.
|
At 12 months’ follow-up, 22 eyes remained in the MMC group, and 23 remained in the MMC–Ologen group. In the MMC group, IOP was 25.96 ± 4.82 mm Hg preoperatively and dropped to 11.33 ± 3.81 mm Hg postoperatively. In comparison, preoperative IOP in the MMC–Ologen group was 26.32 ± 4.27 mm Hg; this dropped to 14.35 ± 3.34 mm Hg postoperatively. Greater IOP reduction was noted in the MMC group at the 6- and 12-month marks (56.9% and 55%, respectively) than in the MMC–Ologen group (47.1% and 44.2%). When an IOP of ≤15 mm Hg was considered as the definition of success, cumulative success was achieved in 86.5% of MMC eyes and in 73.9% of MMC–Ologen eyes.
Medication outcomes were similar between the 2 groups at the 12-month mark—17 of the 22 remaining patients in the MMC group were off glaucoma medications at this point, versus 18 of the 23 in the MMC–Ologen group. Similarly, no significant differences were noted between the 2 groups in terms of complication rates.
The authors stated that, given the homogenous nature of their patient population, the implant should be evaluated in a more heterogenous population with different ethnicities represented. Nonetheless, they said, despite the theoretical advantages of the implant, it appears to offer no practical advantage.
The original article can be found here.