Download PDF
Open globe injuries are a significant cause of permanent visual impairment and ocular morbidity worldwide. Prompt assessment of the type and extent of the injury is critical to ensure timely management.
Etiology and Terminology
Open globe injury (OGI) is defined as a full-thickness wound of the eyewall, due to either a laceration or an occult rupture.1 Classically, a ruptured globe occurs when a considerable amount of blunt force is applied to the eye. This force causes a rapid elevation of intraocular pressure (IOP) that leads to frank rupture of the eyewall by means of an inside-out mechanism.
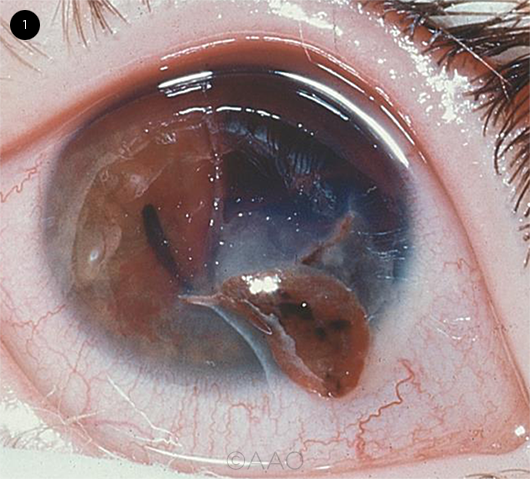
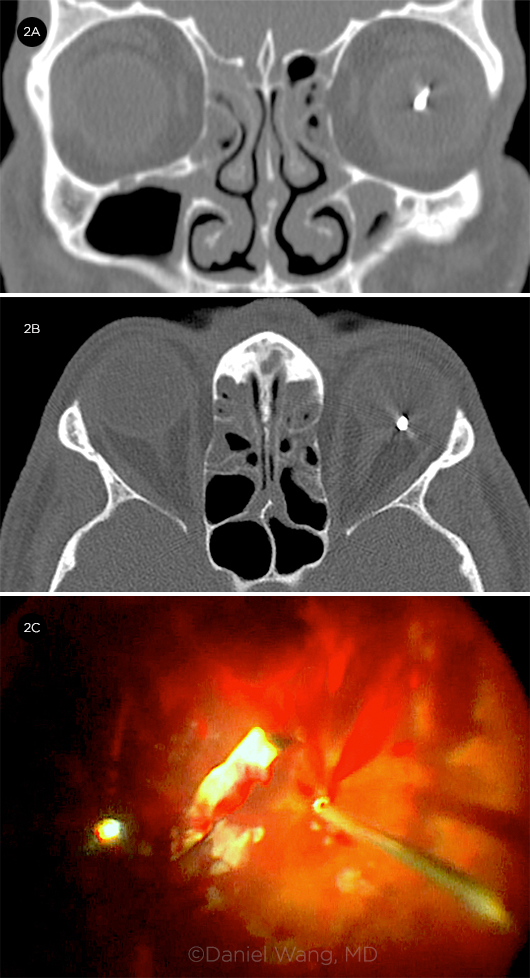
Lacerating injuries are full-thickness disruptions of the eyewall that are caused by external trauma, usually by a sharp object (Fig. 1). These injuries are further subdivided into penetrating, perforating, and intraocular foreign body (IOFB) trauma (Fig. 2).1 Penetrating trauma has an entry point into the globe but no clearly defined exit wound, whereas perforating ocular injuries have both entrance and exit wounds through the eyewall.
Zones. The anatomic region, or zone, of an OGI is an important prognostic factor for visual potential.
Zone I trauma involves the cornea and limbus.
Zone II extends posteriorly from the limbus up to 5 mm posterior to the limbus; these injuries usually involve deeper structures of the anterior segment, including the lens and zonules.
Zone III trauma extends more than 5 mm posterior to the limbus, involving the posterior segment (e.g., the retina, optic nerve, and choroid).2
 |
|
OPEN GLOBE INJURY. Full-thickness corneal laceration, with iris prolapse through the wound.
|
Epidemiology
The worldwide incidence of OGI has been estimated at 3.5 injuries per 100,000 persons, with more than 203,000 cases occurring each year.2 Men and boys make up approximately 80% of patients with OGI, with those aged 10 to 30 years being at greatest risk.3 Young men are more likely to sustain perforating or penetrating injuries, particularly during occupational activities.
 |
|
INTRAOCULAR FOREIGN BODY. (2A) Coronal and (2B) axial CT images show an IOFB in the patient’s left eye. (2C) Removal of the same metallic IOFB.
|
Evaluation
Presentation. When a patient presents with ocular trauma, the clinician should first evaluate for life-threatening injuries. If necessary, the patient should be triaged and sent to the nearest trauma center and/or stabilized. Potentially lifesaving procedures and surgery take priority over ocular assessment and treatment. When the patient is stable, an ocular evaluation can proceed to determine the magnitude of the ocular injury and its subsequent management.
History. It is critical to determine when the injury occurred, as repair should ideally be conducted within 24 hours of the trauma. Details of the circumstances are important. For example, the involvement of a sharp object, high-impact blunt trauma, or high-velocity projectiles should raise the suspicion of an OGI. Where the injury took place is also pertinent because contamination of the wound with soil or organic matter is more likely in rural or agricultural settings.
The initial symptoms following the trauma should be noted, as well as any significant changes such as increasing pain or worsening vision, which could indicate the development of endophthalmitis. A thorough review of the patient’s past ocular and surgical history is important in evaluating the visual potential; moreover, prior surgical sites may be predisposed to rupture. If surgery is contemplated, it is necessary to determine when the patient last consumed food or liquids.
External exam. Care should be taken to minimize manipulation of the globe whenever an OGI is suspected. Inspection starts with an external assessment of the head, face, eyelids, and periocular regions to note any ecchymosis, edema, or superficial lacerations that may be present. Facial asymmetry or bony discontinuities are suggestive of concurrent facial fractures.
If protruding foreign bodies are seen, they should not be removed until the patient is in the controlled conditions of the OR. Additionally, any eyedrops administered should come from a new, sterile bottle.
Visual acuity and pupils. Measurement of visual acuity is necessary to establish a baseline for future visits and to prognosticate visual outcomes.
Pupillary examination may reveal subtle clues about the extent of injury. A dilated pupil may indicate traumatic mydriasis, iris sphincter damage, or possible third nerve palsy. A peaked pupil is often considered pathognomonic for OGI. A relative afferent pupillary defect is suggestive of severe optic nerve damage or retinal injury.
IOP. Measurement of IOP should be delayed until an OGI is ruled out to avoid further damage and extrusion of intraocular contents. In general, hypotony is highly suggestive of OGI; however, a normal IOP does not eliminate the possibility of OGI.
Slit-lamp studies. The slit-lamp exam should include a detailed inspection of the conjunctiva and sclera. Subconjunctival hemorrhage and chemosis may hide underlying scleral lacerations. Eyelid eversion may be performed carefully, and the fornices swept gently for retained foreign material.
All layers of the cornea should be thoroughly inspected for superficial abrasions, edema, and lacerations. A Seidel test is required to evaluate the thickness of identified lacerations. The anterior chamber should be assessed for uniform depth, the presence of cells, flare, hyphema, and vitreous.
The iris should be examined for tears or breaks by both direct and retroillumination. Lens position and clarity and the integrity of the lens capsule and zonular fibers should be evaluated.
Finally, the posterior segment should be examined for the presence of hemorrhage, retinal or choroidal detachment, and possible IOFBs.
Diagnostic imaging. In cases where ocular examination is limited, ancillary imaging studies are recommended to aid in the structural evaluation of the eye and to rule out the presence of a foreign body.
Computed tomography (CT). Noncontrast orbital CT is the recommended imaging modality for ocular trauma and should be employed for most patients with a suspected OGI. Globe contour, abnormality of the lens, vitreous hemorrhage, retinal detachment, orbital and facial fractures, and obvious orbital volume loss can all be assessed with this modality. CT scans have a reported sensitivity between 56% and 68% in diagnosing patients with an open globe.4 Most important, CT is particularly useful if a metallic IOFB is suspected, in which case magnetic resonance imaging is contraindicated.
Although plain film x-ray may be used to screen for the presence of a metallic IOFB, it lacks CT’s ability to identify radiolucent material and soft tissue. Thus, it is not the optimal imaging modality for OGI.
Ultrasonography. B-scan ultrasonography may be useful in providing information about the posterior segment, particularly when the funduscopic examination is limited by hazy media resulting from significant hemorrhage or corneal edema. In some cases, the presence and location of an IOFB may be identified. Care should be taken to avoid pressure on the globe from the probe; however, in many cases, this modality is not recommended prior to globe repair.
Preoperative Management
In anticipation of possible surgery, patients should be kept on NPO status (no food or liquids by mouth). The eye should be covered with a protective shield at all times to prevent further injury. In general, topical ointments should be avoided, although topical nonpreserved antibiotics may be used if there is a delay in getting the patient to the OR. Treatment may be given for nausea (ondansetron 0.15 mg/kg per dose, up to 12 mg IV) and severe pain (morphine, 0.1 mg/kg per dose, up to 10 mg), ideally with IV medications.
Antibiotics. Endophthalmitis is a potentially devastating complication after OGI. The rate of endophthalmitis following OGI has been reported to be higher in patients with IOFBs.5 Antibiotic prophylaxis to prevent development of posttraumatic endophthalmitis has become common practice. Although standardized guidelines for antibiotic selection and route have not been established, there is strong evidence to support the use of 48 hours of IV therapy.6 Gram-positive cocci, gram-positive and gram-negative bacilli, and fungi are the most common organisms isolated in culture-positive cases of endophthalmitis after trauma.7
Broad-spectrum antibiotics are needed to provide coverage for both gram-positive and gram-negative bacteria. IV vancomycin (15 mg/kg; maximum dose, 1.5 g) and a third-generation cephalosporin such as ceftazidime (50 mg/kg; maximum dose, 2.0 g) may be given. Unless there are high-risk features such as intraocular organic foreign material, prophylactic antifungal coverage is not routinely given.
The use of intravitreal antibiotics is controversial in the absence of endophthalmitis, unless there is delayed primary closure or presence of an organic IOFB.8
Tetanus prophylaxis. Although rare, cases of posttraumatic endophthalmitis caused by Clostridium tetani have been reported in the literature. Tetanus prophylaxis may be considered after perforating or penetrating globe injury, particularly when the patient’s immunization status is unknown or not up to date. In addition, tetanus immune globulin may be administered on an individual case-by-case basis.
Prognosis
The mechanism and extent of initial injury and findings at presentation are important predictors of final outcome. To establish an objective, standardized system for assessment of ocular injuries and prognosis, Kuhn and colleagues developed the Ocular Trauma Score (OTS) from an analysis of 2,500 eye injuries.9 The OTS can be easily calculated following the initial examination or surgery and can assist in clinical decision-making and patient discussion. The OTS is a point system based on factors that have strong prognostic significance. These include initial visual acuity as well as the presence of globe rupture, perforating injury, IOFB, endophthalmitis, retinal detachment, or relative afferent pupillary defect.9 Zone III and ruptured globe injuries carry a statistically significant poor prognosis.10
Surgical Considerations
As a general principle, primary globe repair should be completed within 24 hours of injury and evaluation. Either a staged or comprehensive surgical approach may be taken.
In a staged surgical strategy, the primary surgery addresses proper wound closure, management of any prolapsed tissue, and removal of blood and foreign material in the anterior chamber to permit an adequate view for subsequent ocular procedures. Secondary surgeries (such as vitrectomy) are planned and performed later, often in collaboration with colleagues.
In a comprehensive surgical approach, all injuries are managed during initial wound repair and closure. Depending on the zone of trauma, this approach may require the ability to manage both the anterior and posterior segments.
There are advantages and disadvantages to both staged and comprehensive approaches. In addition, controversy persists on the ideal timing of the secondary intervention when a staged approach is elected.
Postoperative Follow-up
After surgical repair, the patient should be directed to wear a protective shield at all times, including while sleeping, and be given careful instructions to refrain from rubbing or touching the eye. In addition, the patient should not engage in heavy lifting, exercise, or swimming for at least six weeks.
The use of safety goggles should be strongly encouraged, particularly for patients in occupations that elevate their risk of ocular injury. Further, the patient may require a multidisciplinary team including social work and psychiatry to provide support following definitive repair.
__________________________
1 Kuhn F et al. Graefes Arch Clin Exp Ophthalmol. 1996;234(6):399-403.
2 Pieramici DJ et al. Am J Ophthalmol. 1997;123(6):820-831.
3 Casson RJ et al. Clin Exp Ophthalmol. 2002;30(1):15-18.
4 Arey ML et al. Ophthalmology. 2007;114(8):1448-1452.
5 Essex RW et al. Ophthalmology. 2004;111(11):2015-2022.
6 Andreoli CM et al. Am J Ophthalmol. 2009;147(4):601608.e2.
7 Long C et al. BMC Ophthalmol. 2014;14:34.
8 Mittra RA, Mieler WF. Surv Ophthalmol. 1999;44(3):215-225.
9 Kuhn F et al. Ophthalmol Clin North Am. 2002;15(2)163-165.
10 Fujikawa A et al. BMC Ophthalmol. 2018;18(1):138.
___________________________
Dr. Wang is a third-year ophthalmology resident, and Dr. Deobhakta is clinical assistant professor of ophthalmology; both are at the New York Eye and Ear Infirmary, in New York City. Financial disclosures: None.