By Rebecca Taylor, Contributing Writer, interviewing Mary Beth Aronow, MD, Zélia M. Corrêa, MD, PhD, and Hakan Demirci, MD
Download PDF
Treatment for ocular surface squamous neoplasia (OSSN) isn’t what it used to be. Today, excision-only protocols are being replaced by topical chemotherapy, which may be used by itself or in combination with surgery.
The Limits of Excision Alone
Topical chemotherapy is making inroads in part because excision—using the no-touch technique with 2- to 3-mm margins—is plagued by 2 issues: recurrence rates that range from 5% to a whopping 69% and possible surgical side effects.1,2
Extensive or repeated surgery carries risks, said Zélia M. Corrêa, MD, PhD, at the Wilmer Eye Institute in Baltimore. “If you perform excisional surgery for OSSN repeatedly, you’ll soon run out of tissue and have trouble reconstructing the ocular surface, as surgery induces varying degrees of scarring,” she said. “Forniceal shortening, limitation in ocular motility, and stem cell deficiency are the most dreaded long-term complications.”
 |
|
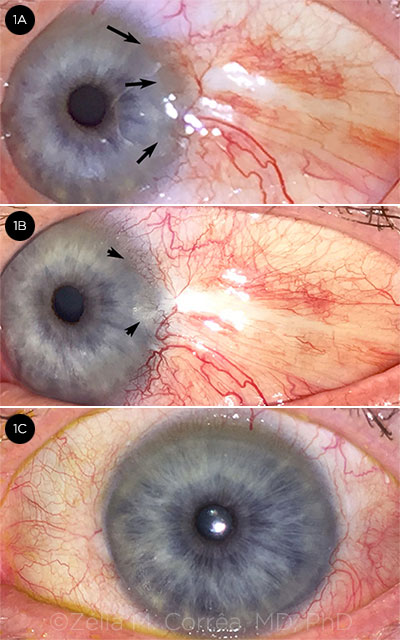
TOPICAL INTERFERON. (1A) Three months after excision of OSSN (intraepithelial squamous neoplasia CIN IV), there are signs of recurrence at the limbus and peripheral cornea (arrows). (1B) Two months into treatment with topical interferon, there is improvement of the gelatinous tissue in the cornea (2 short arrows) but mild increase of conjunctival hyperemia. (1C) After 6 months of topical interferon, there is no visible tumor and the ocular surface is fully healed.
|
Enter Topical Chemotherapy
The most frequently used topical chemotherapies for OSSN are interferon alpha-2b, 5-fluorouracil (5-FU), and mitomycin C (MMC). Interferon alpha-2b is also used for intralesional injections. These chemotherapy agents can be used alone or as adjuvant therapy to excision before, during, or after surgery.1
Treat by subtype. “Topical management of OSSN is primarily for the precancerous CIN [conjunctival intraepithelial neoplasia] subtype of OSSN,” said Hakan Demirci, MD, at the Kellogg Eye Center in Ann Arbor, Michigan (see “What Type Is It?”). “Benign OSSN is treated either surgically or, in some resistant cases, with topical chemotherapy. Squamous cell carcinoma [SCC] is typically treated surgically, with topical therapy for surrounding precancerous areas.”
 |
|
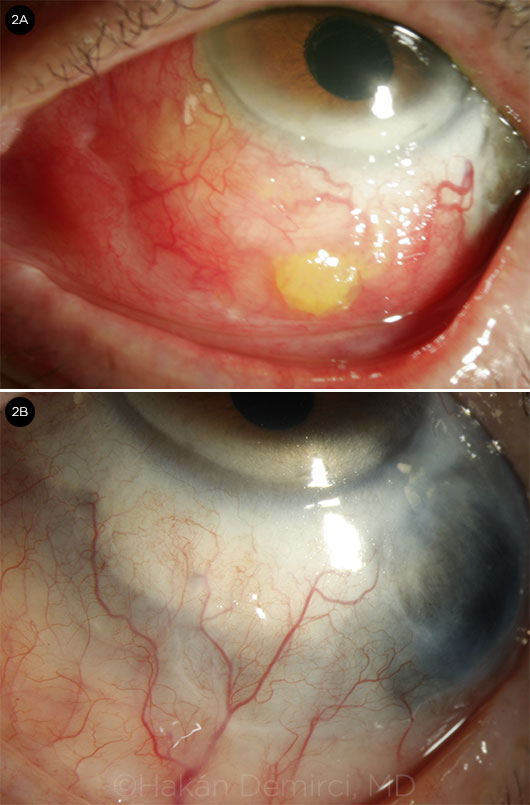
INTRALESIONAL INJECTIONS. (2A) Recurrent OSSN (intraepithelial squamous neoplasia CIN III) involving the entire inferior bulbar and forniceal conjunctiva. Multiple surgical excisions led to scleral thinning. Interferon was injected into the lesion inferiorly and inferotemporally. (2B) After 3 once-monthly intralesional injections, the lesion completely resolved, with no recurrence after 3 years of follow-up.
|
A Look at the Options
To date, no large-scale, randomized clinical trials have compared interferon, 5-FU, and/or MMC. When planning treatment, Drs. Corrêa and Demirci, along with Mary Beth Aronow, MD, at Massachusetts Eye & Ear in Boston, evaluate cases based on the following factors:
- The patient’s age and medical history
- Prior history of scarring or keloid
- Clinical and pathological features of the ocular surface lesion: benign, precancerous, or invasive SCC
- Extent of the lesion and invasion of the fornix
- Condition of the ocular surface, including corneal disease and severe dry eye
- The patient’s likely long-term adherence to topical medication
- The patient’s ability to afford the out-of-pocket cost of topical chemotherapy
Interferon alpha-2b. This is the latest addition to topical chemotherapy, and it also has the fewest side effects. “The newest thing we’re using now is interferon alpha-2b, which is a form of immunotherapy, compounded into eyedrops,” Dr. Corrêa said.
“Our goal is to provide the most effective treatment with the lowest side effect profile,” said Dr. Demirci, “especially for patients who have underlying cornea and conjunctival problems, which is why I like to start with interferon.”
Selected results. One study of interferon as monotherapy found complete remission of tumors in 91.6%, or 22 out of 24 eyes.3 In another study of 89 patients, topical interferon combined with all-trans retinoic acid resulted in 97.8% tumor clearance and tumor-free follow-up after 51.5 months.4
“One of the many advantages of this therapy for patients is that after treatment is started, we don’t need to see them back for 4 to 6 weeks since the rates of toxicity and complications are so low,” Dr. Corrêa said.
Use. Interferon must be refrigerated, and patients have to use the drops 4 times a day for 6 months, said Dr. Corrêa. She noted that taking the full course is critical, as any lingering microscopic disease places the patient at risk of recurrence.
“The key is patient buy-in, because if patients don’t fully comply, you won’t obtain good results,” Dr. Corrêa said. She reported a case in which 1 of her patients returned 6 weeks after starting topical interferon—and the ocular surface tumor hadn’t changed. The patient admitted, “The medication is so expensive, I decided to [use it] just twice a day.”
Drops plus injections. Intralesional injections of interferon are now being used either alone or in combination with interferon drops for some patients.
“I give intralesional injections of interferon once monthly into the area where OSSN is present,” Dr. Demirci said. “Some patients, unfortunately, can’t afford to pay out-of-pocket for topical medications, but insurance will often cover the cost of intralesional injections.”
5-FU. All 3 ocular oncologists agreed that, of the 2 older topical options, topical chemotherapy with 5-FU is usually better tolerated than MMC.
Selected results. A retrospective study in 2016 using topical 5-FU as primary therapy in 44 patients found complete resolution of OSSN in 82% of patients; nasal location was noted as a risk factor for lack of response.2
Use. “As a treatment for OSSN, 5-FU is inexpensive, it works, and it doesn’t need refrigeration,” said Dr. Aronow. “Patients typically take the eyedrops 4 times a day for 4 to 7 days, then [they] take 1 to 3 weeks off before starting the next cycle. Patients are not taking the drops continuously, and this alleviates some of the toxicities associated with therapy.”
MMC. “MMC may be more potent [than 5-FU] but is not as well tolerated, so I generally reserve this for larger or more aggressive lesions that have failed other therapies,” said Dr. Aronow.
Selected results. Several studies have shown successful treatment with 0.02% or 0.04% topical MMC 4 times a day prescribed for 1 to 4 weeks and repeated as necessary.1
Use. MMC has some clear disadvantages. “MMC causes a lot of irritation, redness in and around the eye, even some corneal problems,” said Dr. Demirci, “so we warn patients about side effects and watch them carefully with more frequent follow-ups.”
“Because patients have to be seen more frequently to monitor for toxicity, there may be additional cost considerations, such as hospital charges for extra clinic visits and transportation to visits,” Dr. Aronow said. “With these added cost factors to consider, it can be challenging to directly compare the cost of 1 therapy over another.”
MMC plus interferon. “In some cases,” noted Dr. Corrêa, “a combination of these drugs can be more effective [than any single drug alone].” In a 2018 pilot study of 6 patients with MMC-resistant OSSN, for instance, all tumors completely resolved after 24 weeks of topical interferon.5
What Type Is It?
OSSN covers a spectrum across 3 subtypes: benign dysplasia, precancerous conjunctival intraepithelial neoplasia (CIN), and malignant squamous cell carcinoma (SCC).
Diagnosis. OSSN is more common in men, people who work outdoors, and patients with the human immunodeficiency virus (HIV). With regard to the latter, a retrospective study of OSSN concluded that the condition may be the first symptom of HIV infection.1
“When diagnosing OSSN,” said Dr. Aronow, “typical clinical features include a gelatinous-appearing lesion with leukoplakia and prominent (feeder) blood vessels. While OSSN can frequently be identified clinically, histopathology is necessary to confirm definitively where the lesion falls on the OSSN spectrum.”
___________________________
1 Dandala PP. J Clin Diagn Res. Published online Nov. 1, 2015.
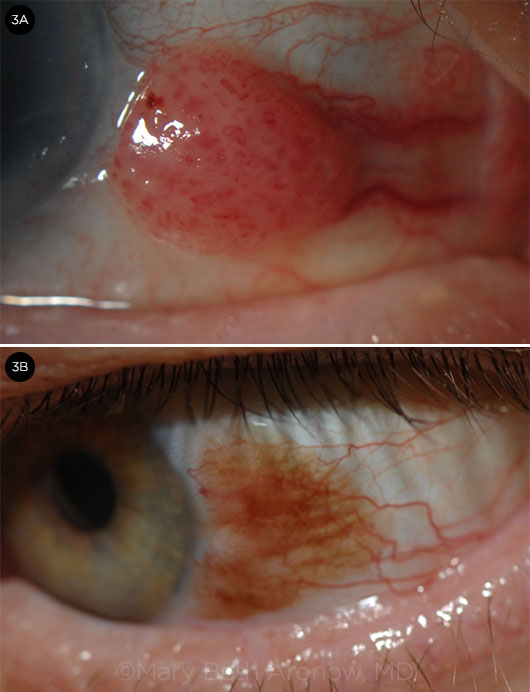
PRESENTATION. (3A) Gelatinous conjunctival OSSN involving the nasal bulbar conjunctiva of the right eye, with frond-like vasculature within the mass and prominent associated feeder vessels. (3B) A pigmented conjunctival lesion with prominent vascularity revealed pigmented squamous cell carcinoma.
|
Additional Options
What about cidofovir? “If you have a patient with recurrent or refractory OSSN and you feel you’re exhausting your options, try to evaluate the biopsy specimen with a PCR-based test to assess for the human papillomavirus [HPV],” Dr. Corrêa advised. “These refractory cases may have an underlying infection that most ophthalmologists are not aware of and patients may not report.”
When HPV is confirmed, the antiviral drug cidofovir “has shown very promising results,” Dr. Corrêa said, and she noted that a recent report showed roughly 6.5% of OSSN specimens were positive for HPV-16.4
“Viruses might play a role in the pathogenesis of OSSN,” Dr. Demirci agreed, “and antiviral medications have been used in different parts of the world with interesting results, although these are observational reports with a limited number of cases.”
What about anti-VEGF drugs? Some ocular oncologists are now trying anti–VEGF (vascular endothelial growth factor) medications for OSSN.
“Some doctors are claiming they had a good response with bevacizumab eyedrops [for OSSN], but it’s a very small number of cases,” Dr. Corrêa said. Dr. Demirci added, “Anti-VEGF therapy has been tried in some cases, but the results are not as effective as with interferon.”
Topical Treatment at a Glance
| Medication |
Concentration |
Regimena |
Duration |
Common Side Effects |
| Chemotherapeutic |
| Interferon alpha-2b1 |
1 million IU/mL |
4 times daily |
5 months |
Mild papillary conjunctivitis; epithelial mycrocysts; marginal keratitis |
| MMC2 |
0.02% or 0.04% |
4 times daily |
1-4 weeks; repeat as needed; usually multiple interrupted 1-week courses |
Conjunctival hyperemia; burning sensation; punctate keratitis; lid toxicity; epiphora/punctal stenosis |
| 5-FU2 |
1% |
3-5 times daily |
4 weeks, or 2 interrupted courses of 2 weeks each |
Same as those noted with MMC, but milder |
| Other |
| Bevacizumab3 |
5 mg/mL |
4 times daily |
8 weeks |
None reported |
| Cidofovir4 |
2.5 mg/mL |
3 times daily, continued until tumor is clinically invisible + 1 week |
454 days (range, 222-876 days) |
Conjunctivitis; punctal stenosis |
| Retinoic acid1 |
0.01%/mL |
1 drop every other day |
While using interferon |
Not known |
|
a Interferon and retinoic acid are used together.
1 Krilis M et al. Ophthalmology. 2012;119(10):1969-1973.
2 Pe’er J. Int Ophthalmol Clin. 2015;55(1):9-21.
3 Asena L et al. J Ocul Pharmacol Ther. 2015;31(8):487-490.
4 Ip MH et al. Ophthalmology. 2018;125(4):617-619.
SOURCE: Zélia M. Corrêa, MD, PhD
|
Punctal Stenosis: To Plug or Not to Plug?
One final note: If scarring and stenosis of the punctum occurs as a result of topical treatment, chronic tearing may result.
“When using topical chemotherapies, some physicians use punctal plugs to help prevent [potential] stenosis,” said Dr. Aronow, “while others favor allowing the drops to have access to the punctum to treat potential microscopic disease there. I prefer to use punctal plugs because, although rare, punctal stenosis can be difficult to treat and is relatively easy to prevent.”
___________________________
1 Pe’er J. Int Ophthalmol Clin. 2015;55(1):9-21.
2 Joag MG et al. Ophthalmology. 2016;123(7):1442-1448.
3 Kusumesh R et al. Asia Pac J Ophthalmol. 2015;4(5):279-282.
4 Ip MH et al. Ophthalmology. 2018;125(4):617-619.
5 Singh M et al. Int Ophthalmol. Published online Jan. 23, 2018.
___________________________
Dr. Aronow is assistant professor of ophthalmology at Harvard Medical School and assistant scientist at Massachusetts Eye & Ear in Boston. Financial disclosures: None.
Dr. Corrêa is the Tom Clancy Endowed Professor of Ophthalmology at the Wilmer Eye Institute in Baltimore. Financial disclosures: Castle Biosciences: C.
Dr. Demirci is associate professor of ophthalmology and visual sciences and director of Ocular Oncology at the Kellogg Eye Center in Ann Arbor, Mich. Financial disclosures: Castle Biosciences: C.
See the disclosure key at www.aao.org/eyenet/disclosures.