Download PDF
Phacoemulsification and IOL implantation alone—without concurrent glaucoma surgery—appears to be a reasonable and safe surgical option for certain glaucoma patients whose disease is well controlled with 1 or 2 medications.
According to a recent Academy Ophthalmic Technology Assessment (OTA), the available published evidence supports the phaco-only approach for well-controlled cases of primary open-angle glaucoma (POAG), including normal-tension cases (NTG), pseudoexfoliation glaucoma (PXG), and primary angle-closure glaucoma (PACG).1
“You don’t have to see every patient who comes to you with both a cataract and glaucoma as a candidate for combined surgery,” said coauthor Philip P. Chen, MD. “From the evidence that we have, for people who are not poorly controlled, for people who are not on a maximum medications, doing the cataract surgery alone is a reasonable option. It’s quite safe.” Dr. Chen is professor and Grace E. Hill Chair in Vision Research at the University of Washington, in Seattle, and chief of ophthalmology at the UW Medicine Eye Institute.
Phaco effects. The OTA panel found that when IOP was under good medical control before phaco:
- Postop decreases in mean IOP were “small” and “moderate” in POAG and PXG eyes (–13% and –20%, respectively) and “substantial” (–30%) in PACG eyes.
- On average, medication use after the cataract surgery fell by 12% in POAG eyes, 35% in PXG, and 58% in PACG. (The latter group included eyes that were poorly controlled before phaco.)
- Pre-phaco IOP was the factor that most consistently influenced the amount of IOP reduction; the higher the IOP, the greater the IOP reduction.
- Worse IOP control after phaco was reported in up to 14% to 26% of patients, but few patients subsequently required filtration surgery (0%-4%) 1 to 5 years after cataract surgery.
- An early IOP spike occurred in some patients (median, 8%-21%, depending on the glaucoma type), but it was transient and usually manageable with medication.
Limitations. The panel’s review encompassed the best available knowledge through late 2014, but the process also highlighted gaps and limitations in the evidence, Dr. Chen said.
“One problem for us was that we had relatively few studies to draw upon because combined phaco and glaucoma surgery has typically been considered the standard of care. In addition, a lot of the papers were retrospective, were not well controlled, and had methodological problems,” Dr. Chen said. “We certainly could use better quality evidence in this area.”
Safety of phaco alone. Despite the limitations, the OTA panel found sufficient evidence to identify POAG (including NTG), PXG, and PACG as the glaucoma patient groups that can be routinely spared from combined phaco/filtration procedures, Dr. Chen said. These constitute the majority of glaucoma patients that ophthalmologists generally encounter, he said.
“I think that the average ophthalmologist can be assured that for the vast majority of their patients with one of these types of glaucoma, which is controlled on 1 or 2 medications, doing cataract surgery alone will not be dangerous for the patient,” Dr. Chen said. “It’s safe to do the cataract surgery alone.”
—Linda Roach
___________________________
1 Chen PP et al. Ophthalmology. 2015;122(7):1294-1307.
___________________________
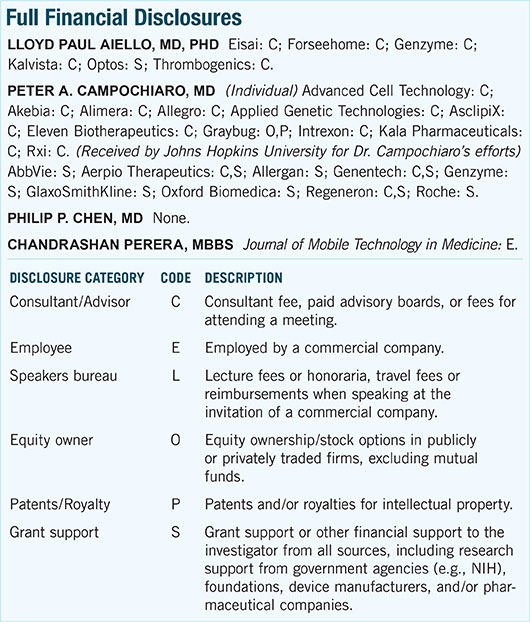
Relevant financial disclosures: Dr. Chen—None.
For full disclosures and disclosure key, see below.
More from this month's News in Review